Abstract
Cortical bone trajectory (CBT) screw was firstly utilized by Santoni in 2009, which had been proved to have stronger hold force, especially in the osteoporosis vertebrae compared with the pedicle screw (PS). In this study, we developed a technique combining pedicle screw, cortical bone trajectory screw, and sacral alar screw, which was named as multiple trajectory anchoring (MTA) technique for patients who underwent lumbar-sacral fusion. The technique comes with the following improvements and advantages. First, the satellite rods are fixed with the additional screws which makes the tension more dispersed and avoids stress concentration. Second, the interaction between the multi-trajectory screws anchoring on one vertebra makes the screws stronger and reduce the risk of screw loosening. Third, the MTA screw can provide better stability for the anterior column. Forth, the MTA fixation can not only strengthen the construct, but also provide additional correction force. In this chapter, we aimed to introduce an original lumbar-sacral strengthening technique, multiple trajectory anchoring(MTA), for lumbar-sacral fusion. It is a safe and effective means to strengthen lumbar-sacral internal fixation as well as provide additional correction force for patients with lumbar-sacral degeneration, deformity and tumor. More importantly, it provides an alternative solution for pelvic fixation.
Keywords
- cortical bone trajectory
- pedicle fixation
- lumbar fusion
- multiple trajectory anchoring fixation
- spinal fixation
1. Introduction
Pedicle screws (PS) are the most common method of sacral fixation. Spinal fusion with traditional bilateral PS fixation has been described for a variety of surgical indications, such as spinal canal stenosis, spinal degenerative disc disease, spinal slip, spinal tumor, spinal trauma, and malformations [1, 2, 3, 4, 5]. However, the main defects of the sacral PS fixation are screw loosening and pseudarthrosis, especially in the long-segment surgery and in fixation for osteoporotic patients. While a percutaneous pedicle screw (PPS) technique is an alternative, it requires an additional method of decompression and bone grafting. In addition, the PPS technique relies on intraoperative multiplanar fluoroscopy, which leads to high radiation exposure risk for surgeons and patients. In addition, screw loosening is known to be a complication of PS fixation, especially in osteoporotic patients. There are several methods to enhance the purchase of screws, such as modifying screw design and strengthening the vertebrae with augmentation materials or the combination of cortical pedicle screw techniques. However, they remain unavailable for severe osteoporosis. Weaknesses of bone cement include its high exothermic polymerizing temperature, high monomer toxicity, and high risk of cement leakage into vertebrae. Cortical bone trajectory (CBT) screw was first utilized by Santoni [6] in 2009, which had been proved to have stronger hold force, especially in the osteoporosis vertebrae, compared with the pedicle screw. In 2013, Masaki [7] put forward the double-trajectory technique, cortical bone trajectory combined with traditional pedicle trajectory, in a patient with degenerative lumbar scoliosis and osteoporosis. We developed a technique combining pedicle screw, cortical bone trajectory screw, and sacral alar screw, which was named as the multiple trajectory anchoring (MTA) technique, for patients who underwent lumbar-sacral fusion (Figure 1). It provided an alternative solution for pelvic fixation and kept the motion of sacroiliac joint in the lumbar-sacral fusion surgery. With the MTA technique, CBT screws were selectively implanted in the lumbar spine and sacral alar screws were inserted on the same side of the sacrum, after completing the pedicle screw fixation and interbody fusion. And the screws were then connected with titanium or cobalt rod(s), which increased the strength of the internal fixation and provided additional strength for compression or distraction.
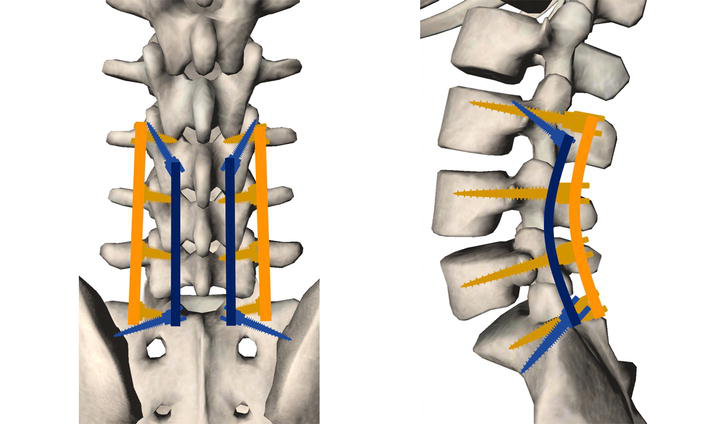
Figure 1.
The schematic diagram of the multiple trajectory anchoring (MTA) technique. Pedicle screws are in yellow. CBT and sacral alar screws are in blue.
2. Anatomy and biomechanics of the MTA technique
As described by Masaki [7], the combined application of the CBT and PS in the same vertebrae was safe and feasible. The entry point of CBT screw was the intersection point of the vertical line at the midpoint of the superior articular process and a line 1 mm below the inferior edge of the transverse process. CBT screws rely on 4-point purchase between the dorsal cortex at the site of insertion, the medial and lateral cortex of the pedicle wall, and the curvature of the vertebral body wall, to maximize the cortical bone contact to improve purchase strength. The CBT screw followed a caudal-to-cephalad path in the sagittal plane and a medial-to-lateral path in the transverse plane through the pedicle, which maximized the thread contact of the screws with the vertebral cortical bone and offered stronger fixation strength. In the MTA technique, the sacral alar screw is inserted additionally based on the PS fixation and connected with the cranial CBT screw to enhance the fixation and reduce the incidence of pseudarthrosis. The entry point of the sacral alar screw is in the lower edge of the L5-S1 articular process, which is medial to the pedicle screw and can be well aligned with CBT screws. The outreach angle is 35 to 45 degrees and the sagittal inclination angle is 30 to 35 degrees. The length of the sacral alar screw can range from 35 to 45 mm. Breaking through the ventral cortical bone can maximize the anti-pullout strength. With the MTA technique, CBT screws were selectively implanted in the lumbar spine and sacral alar screws were inserted on the same side of the sacrum, after completing the pedicle screw fixation and interbody fusion. And the screws were then connected with titanium or cobalt rod(s), which increased the strength of the internal fixation and provided additional strength for compression or distraction.
Santoni found that CBT screws and PS have comparable pullout strengths and switching characteristics. Compared to PS, CBT screws showed a 30% increase in uniaxial pullout strength. However, the traditional pedicle trajectory screws are different from CBT. It is unclear whether screws and trajectory affect the uniaxial pullout strength of a single axis. Ueno studied the relationship between thread screw entry trajectory or thread characteristics and pullout strength in pig cadaver experiments. The results showed that the cortical screw was able to improve fixation strength but not significantly improve pullout strength. This specific trajectory appeared to have a major impact on pullout force. The biomechanical properties of PS and CBT screws were investigated by Calvert in which each screw was used to rescue the other in the setting of revision in 10 fresh-frozen human lumbar spines. The results of this study showed that CBT rescue screws retained 60% of the original pullout strength of PS, while traditional salvage screws retained 65% of the original CBT screw pullout strength. Either CBT or PS use as a rescue choice in the setting of a failed or compromised pedicle screw construct in the lumbar spine is supported by it. Baluch found that the CBT screw had greater loosening resistance in the fatigue tests when compared to the PS. According to Perez-Orribo, there was no significant difference in the mean range of motion or area of laxity of the CBT screw and PS during any mode of loading. Matsukawa [8] reported that CBT screws have 2.01 Ncm (Newton centimeter units) higher insertion torque than PS in vivo. CBT screw’s fixation strength is superior to those of the traditional pedicle screws, as loading the flexing and stretching load resistance is higher, but its ability to fight the lateral bending and axial rotation is poorer. The mechanical performance of the CBT screw is attributed to such factors as the position of the screw specifications, placement, and patient’s bone. One of the most critical factors is the size and length of the screw, the factors in the subsequent have also been confirmed in the experiments of other relevant bodies [9]. Compared with the traditional technique of pedicle screws, the use of CBT of bigger size and length can enhance biomechanical properties of the screw. Xiao-yu wu et al. [10] established a finite element model through a case of osteoporosis, simulated traditional pedicle screw and CBT screw in a two-way fixed effect. The results suggested that the stability of CBT group under flexion extension and rotation was greater than that of conventional pedicle screw group; extension and rotation was greater than that of conventional pedicle screw group; The CT values of the CBT group nail way around the bone are greater than conventional pedicle screws. The CBT screw technology is one of the preferred methods for lumbar internal fixation in patients with osteoporosis. CBTS internal fixation technology provides biomechanically stronger pullout forces and yield loads, and has similar flexion and extension resistance to PS. The screwing torque is about 1.7 times that of traditional PS internal fixation technology, but it has poor effect on lateral bending and axial rotation resistance. The results of biomechanical experiments and finite element analysis showed that the biomechanical properties of multi-trajectory screw internal fixation were significantly better than those of traditional PS internal fixation. Under the condition of simulating real human movement, multi-trajectory screw internal fixation technique can increase the strength of internal fixation, thereby improving the stability of lumbar fusion segment, reducing the risk of loosening of internal fixation and the incidence of pseudarthrosis, and improving the success rate and satisfaction of surgery. CBTS internal fixation technique can fully protect the posterior paravertebral muscles and facet joints of the spine to avoid postoperative paravertebral atrophy and facet joint degeneration. In addition, the combined application of CBTS internal fixation technique, SAS internal fixation technique, and PS internal fixation technique in lumbar fusion surgery can further increase the mechanical strength of the surgical segment, while obtaining a similar intervertebral stress environment, and effectively increase the mechanical stability of the surgical segment.
The MTA technique we are reporting on has the following biomechanical characteristics. First, compared with the existing multi-rod construct technique, the satellite rods in MTA are fixed on the additional screws that make the stress to be more dispersed and avoid stress concentration. Second, the interaction between the multi-trajectory screws anchoring on one vertebra makes the screws stronger and reduces the risk of screw loosening. Third, the MTA screw can provide more stability to the anterior column and help in interbody bone healing. Fourth, in the lumbar sacral deformity cases, MTA fixation could not only strengthen the construct, but also provide additional correction force to restore both coronal and sagittal balance. Fifth, the MTA technique is based on the usage of CBT screws and sacral alar screws, which provides an alternative for pelvic fixation and preserves the movement of sacroiliac joints. As we know, pelvic fixation may cause dysfunction and even seriously affect the patients’ quality of life. With the application of the MTA technique, pelvic fixation can be reduced and the sacroiliac joint can be preserved. The MTA technique provides additional orthopedic strength and makes the lumbosacral internal fixation more solid. Meanwhile, CBT screw and sacral wing screw insertion through a medial entry point demands no additional exposure of the wound. When inserting the CBT screw, it may cross with pedicle screw, so there are three points to be noted. First, the insertion point of the pedicle screw should be lateral and close to the lower part of the pedicle, so as to leave enough space for the CBT screw. Second, CBT screws should be thinner and shorter than pedicle screws, generally 4.5 mm in diameter and 3.0 mm in length. Before CBT screws are inserted, probe detection can be applied to ensure that the inner wall of the vertebral pedicle is not breached. Third, if the pedicle is too thin to hold two screws, do not proceed with the insertion by force, and the alternative vertebrae can be selected as the upper hook point.
3. Clinical application of the MTA technique
Recent years have seen an increase in the incidence of lumbar degenerative disc disease (DDD) in older adults. There are significant changes in spinal anatomy and curvature with age. Hegazy [11] confirmed changes in the shape and size of lumbar kyphosis in older adults and recommended that more attention be paid to anatomy and curvature during surgery. Furthermore, osteoporosis is fairly common in older people. For this reason, another key treatment strategy for lumbar DDD in older adults is osteoporosis management. In the elderly, osteoporosis may cause loosening of internal fixation. One study reported a pedicle screw loosening rate of 12.8–25% in osteoporotic patients. Furthermore, the risks of both proximal and distal junctional kyphosis also rise as a result. Thus, internal fixation stability in patients with osteoporosis should be improved intraoperatively by employing expansive pedicle screws, bone cement screws, or cortical bone path screws. Expansive pedicle screws can increase the intensity of internal fixation, but there are obvious shortcomings such as complicated placement, high rate of screw breakage, and limited clinical applicability. Compared to the traditional technique, CBT increases the area of contact between the screws and the cortical bone, and all of the screws used in the CBT technique are encircled by cortical bone. Thus, this technique is best suited to the treatment of lumbar DDD patients with osteoporosis. In addition, in 2014, Mizuno proposed the combination of this technique with posterior lumbar midline fixation and fusion in lumbar midline fusion surgery (MIDLF). The CBT technique in MIDLF surgery has been used extensively in cases of lumbar DDD, adjacent spinal disease, and postoperative revision because of its poor invasiveness and high-safety advantages. Recently, with the widespread application of internal fixation of the spine, the incidence of failed back surgery syndrome and autism spectrum disorder (ASD) has increased, resulting in a high proportion of lumbar revision surgeries [12]. The risk of nerve structure and blood vessel exposure is significantly increased in revision surgery due to hypertrophic scar tissue and imprecise spinal anatomy. Minimizing exposure risk in revision surgery is another benefit of the MTA technique. During revision surgery, when the adjacent segment is decompressed and fixed, the internal fixation of the original operation usually needs to be replaced. However, internal fixation replacement may not only increase operative time and surgical risk, but also lead to more blood loss. As a result, decompression, fixation, and fusion on adjacent segments without removal of internal fixation from the original surgical procedure has become a key technique in the treatment of ASD. The CBT technique, which has a single-entry site and trajectory, allows for decompression, complete screw placement, and fusion of adjacent segments through a small incision while preserving the original internal fixation, thus avoiding significant dissection and reducing operative time and surgical risk. For example, the MTA technique can be used to place two groups of screws within the same vertebral body [13]. In a study by Takata et al. [14], it was shown that the CBT technique combined with MIDLF in lumbar revision surgery has the benefits of less soft tissue damage, less postoperative complications, and improved internal fixation stability compared to traditional revision surgery. Lumbosacral spinal fusion is a common surgical procedure for the treatment of spinal pathologies including degenerative disc disease, lumbar spinal stenosis, malformations, trauma, and neoplasms. Fixation in lumbar fusion requires screws to be inserted into the vertebrae. Traditionally, these procedures have been performed via pedicle screw augmentation of the posterior lumbosacral spine in the manner first described by Boucher in 1959. However, advances in spine surgery and a broader trend toward less invasive procedures have resulted in the development of novel and innovative techniques, which are intended to achieve spinal fixation while causing less damage to the surrounding tissues. The traditional PS approach to lumbosacral spine surgery, which is the current standard of care, requires extensive lateral vertebral dissection for screw placement. In contrast, the CBT procedure requires less soft tissue exposure as screws are placed medially to laterally with a starting point at the junction between the lateral pars interarticularis and superior articular process (1 mm inferior to the inferior border of the transverse process, which was projected at the 5 o’clock orientation in the left pedicle and at the 7 o’clock orientation in the right pedicle). Recent trends have demonstrated a shift toward minimally invasive surgical approaches as opposed to traditional invasive approaches. Since CBT involves less spinal dissection and smaller incisions than PS, of the two approaches, it is considered to be the least invasive. Multi-rod technique has been tried in many centers so as to achieve a more rigid construct [15, 16, 17, 18]. Robert [17] performed a retrospective review for consecutive adult spinal deformity patients who underwent long fusion to the pelvis. He concluded that patients treated with multi-rod constructs had a statistically lower incidence of lumbosacral pseudarthrosis and implant failure than those treated with dual-rod constructs. Seung-Jae et al. [16] compared the radiographic outcomes after the use of a standard 2-rod construct versus similar outcomes after the use of a multiple-rod construct, and they thought that using a multiple-rod construct is an effective method to enhance the stability across 3-column osteotomy site, and further to significantly prevent implant failure and symptomatic pseudarthrosis. Yu et al. [18] retrospectively analyzed a consecutive case of patients with adult spinal deformity who underwent 3-column osteotomy with pelvic fixation. He concluded that additional rods covering the osteotomy site and lumbosacral junction can reduce the incidence of rod fracture following 3-column surgery with pelvic fixation. Meanwhile, biomechanical studies have also proved that accessory rods improved the stability and reduced the motion and rod strain at the osteotomy site [19, 20, 21]. However, according to a systematic review of treatment strategies for the prevention of junctional complications after long-segment fusions in the osteoporotic spine conducted by Murray [22], there is less or insufficient evidence to recommend the use of multi-rod constructs. Moreover, there were also some shortcomings in the multi-rod constructs that need to be modified. First, the accessory rods were linked by side-by-side connectors with the primary rods, which might concentrate more stress on the junction of screws and rods. Furthermore, the application of the connector would increase the possibility of mechanical failure, such as the disengagement of the rod from the connector [23, 24]. Second, the multi-rod constructs mainly increased the rigidness of the posterior column, but the reinforcement for anterior column was not achieved. Andrea [25] considered that the high loads acting on the rods with respect to the physiologic condition could slow down the bone healing at the osteotomy site. Furthermore, according to the study of Tomohiro, the use of multi-rod constructs led to a higher incidence of junctional iliac screw loosening than the use of conventional a two-rod construct, especially for patients with osteoporosis, following the adult spinal deformity surgery.
Degenerative diseases of the spine are a common condition affecting the quality of life of middle-aged and elderly people, affecting about 32–68% of people over 65 years of age [26]. Degenerative scoliosis is among the more complex issues, often with vertebral canal and nerve root canal stenosis, vertebral rotation, intervertebral joint subluxation, and sagittal balance loss due to pathological changes. Among them, the incidence of female is higher than that of male. Due to the degeneration of thoracolumbar segment, it can lead to asymmetric joint space stenosis, small joint hyperplasia, osteophyte formation, yellow ligament hypertrophy and spinal canal stenosis, and even vertebral rotation and intervertebral joint subluxation. The clinical and imaging manifestations are often complicated. The treatment is mainly intended to alleviate symptoms, to improve the function of the spine status, to bring about reconstruction of spinal stability, to restore the spinal sagittal balance, and to handle the individual situation of treatment according to different choices of different surgical strategies. Currently, pedicle screw internal fixation is the preferred surgical method to reconstruct spinal stability and restore spinal sequence, but the patients on the receding side are often complicated with osteoporosis. Simple pedicle screw fixation often results in internal fixation loosening and pseudarthrosis formation. The long-term complication rate of 5-year follow-up has been reported to be about 59%. Adult patients with degenerative scoliosis tend to be aging, more often combined with osteoporosis, at the time of long-segment fixation fusion, there is the possibility of internal fixation loosening, pseudojoint, and other complications. A study by Stanley et al. [27] reviewed internal fixation-related complications in patients over 65 years of age who underwent multi-level spinal fusion surgery for bone weakness. A total of 38 patients were included in the study, all of whom underwent more than five levels of surgery. Follow-up time was greater than 5 years, and the incidence of short-term postoperative complications (less than 3 months, vertebral fracture, pedicle fracture) was about 13%, and the incidence of long-term complications (longer than 3 months) was about 59%, including the failure of pseudarthrosis combined with internal fixation 11%, internal fixation loosening 7%, and pelvic internal fixation prolapse 11%. In a large sample of more than 140,000 people, Lee et al. [28] found that osteoporosis significantly lengthens hospital stay for spinal surgery, increases readmission rates, and increases healthcare costs. Therefore, how to reduce the complications related to internal fixation after spinal surgery in the elderly and improve the intensity of fixation should be paid clinical attention and solved. The common ways to improve the strength of the internal fixation in clinic include increasing screw size, using specially designed expansion screws, and vertebral body bone cement reinforcement, which not only improves the fixed strength, but also increases the probability of complications. In 2009, Santoni et al. proposed the surgical method of fixation with cortical bone trajectory screws to reduce the dependence of screws on bone density [6]. Biomechanical studies have confirmed that cortical bone trajectory screws can significantly improve the fixation strength and stability of internal fixation in osteoporosis samples, and a large number of clinical applications have achieved satisfactory results [8, 9, 29, 30]. Different from thoracolumbar short-segment fixation, the treatment of degenerative scoliosis often requires rotation, compression, and distraction. Finite element analysis found that the anti-rotation ability of cortical bone trajectory screw fixed only in the middle and posterior column could not fully meet the needs of surgery. However, the special screw path of cortical bone trajectory screw allows it to be used as a supplement to the pedicle screw in the same vertebral pedicle. Dual-trajectory internal fixation can significantly improve the strength and stability of fixation [29]. As early as in 2013, Japanese scholar Professor Masaki Ueno et al. [31] reported the case of dual-track internal fixation for the treatment of degenerative scoliosis complicated with osteoporosis. Considering that the patient had severe osteoporosis (T = -4.0), the surgeon adopted L1-S1 dual locus fixation, and the balance of coronal and sagittal plane was restored after surgery. The team of Professor Hu Huiqiang [32], a Chinese scholar, conducted an attempt to correct degenerative scoliosis using a cortical screw satellite rod combined with pedicle screw internal fixation. The team followed 11 patients with degenerative scoliosis who underwent satellite stick surgery with cortical screws for an average of 33 months. There was no significant difference in coronal and sagittal balance at the last follow-up compared with immediately after surgery. It has been confirmed that cortical screw fixation combined with pedicle screw fixation combined with satellite rod orthopedic distal fixation to S1 long-segment lumbosacral fusion can enhance the strength of spinal pelvis fixation and achieve better clinical efficacy in the treatment of degenerative scoliosis. The use of MTA technique in the treatment of degenerative scoliosis with osteoporosis has clear safety and efficacy. Compared with Professor Masaki Ueno’s fixed segmental double-trajectory internal fixation, MTA technique selectively inserts cortical bone screws or sacral wing screws on the basis of pedicle screw fixation, which not only ensures the reliability of internal fixation, but also saves the number of internal fixations and reduces the cost of surgical fixation consumables, thereby reducing in the difficulty of surgery and the occurrence of potential surgical complications. Pedicle screws in combination with cortical or sacral wing screws can provide a variety of options for increasing the strength of fixation in the clinic, and provide an effective fixation method for both the surgeon and the patient in spinal deformity correction surgery with osteoporosis, spinal tumor resection and reconstruction surgery, and long-segment fixation for lumbosacral deformity. In conclusion, multi-trajectory and multi-anchor fixation technique can effectively improve the strength of pedicle screw fixation, and can be safely and effectively applied in the surgical treatment of adult degenerative spinal deformities with osteoporosis.
The main indications of the MTA technique are lumbosacral 3-column osteotomy, multi-level lumbosacral fusion for osteoporotic elderly patients, spondylolisthesis, and lumbosacral coronal imbalance. Based on past experience, distal fixation to the pelvic was recommended in the situation above to get stronger internal fixation and greater orthodontic strength. As we know, pelvic fixation may cause dysfunction and even seriously affect the patients’ quality of life. With the application of the MTA technique, pelvic fixation can be reduced and the sacroiliac joint can be preserved. The MTA technique provides additional orthopedic strength and makes the lumbosacral internal fixation more solid. Meanwhile, CBT screw and sacral wing screw insertion through a medial entry point demands no additional exposure of the wound.
In general, sacropelvic fixation should be considered in any patient with a long construct ending in the sacrum, or patients with associated risk factors for distal fixation loosening or high risk of pseudarthrosis at L5-S1, or those undergoing 3-column osteotomies or vertebral body resections in the low lumbar spine, and those with severe spondylolisthesis or trunk imbalance [33, 34]. High biomechanical load makes the lumbosacral junction difficult to stabilize during fusion and leads to pseudarthrosis and internal fixation failure which are the prevalent complications, and it most commonly occurs at the 3-column osteotomy site or the lumbosacral junction [35, 36]. This reminds us of the need for a more solid instrument to stabilize the L5-S1 junction. The construction of iliac screw and S2AI screw has been the major advancement in spinopelvic fixation, and it demonstrates the excellent biomechanics. However, the drawbacks in the spinopelvic fixation, including iliac screw-associated screw site prominence, wound complication [37, 38], implant loosening [39], and S2AI-associated sacral iliac joints’ violation [40], should be carefully considered. Thus, we are trying to put forward an alternative solution for the pelvic fixation in the lumbar sacral surgery to avoid the complications mentioned above. On the other hand, the MTA technique has its limitations and contra-indications. Such as, it is not suitable for patients with severe coronal or sagittal trunk imbalance, which demands sacroiliac screws to provide greater corrective force, and it is difficult to implant both PS and CBT screws for patients with lumbar pedicle dysplasia.
4. Conclusion
The MTA technique is a lumbosacral augmentation fixation technique that combines cortical bone trajectory (CBT) screw with sacral alar screw fixation based on the traditional pedicle screw fixation construct. CBT screws were selectively implanted in the lumbar spine and sacral alar screws were inserted on the same side of the sacrum after completing the pedicle screw fixation and interbody fusion. And the screws were then connected with rod(s), which increased the strength of the internal fixation. The technique comes with the following improvements and advantages. First, the satellite rods are fixed with the additional screws, which make the tension to be more dispersed and avoid stress concentration. Second, the interaction between the multi-trajectory screws anchoring on one vertebra makes the screws stronger and reduces the risk of screw loosening. Third, the MTA screw can provide better stability for the anterior column. Fourth, the MTA fixation can not only strengthen the construct, but also provide additional correction force. Fifth, the MTA technique provides an alternative for pelvic fixation, which preserves the motion of sacroiliac joints.
In conclusion, the MTA technique is a safe and effective means to strengthen lumbosacral internal fixation as well as to provide additional correction for patients with lumbar sacral degenerative, deformity, and tumor. This technique can also be taken as a remedial measure if the pedicle screws loosen intraoperatively. And it still needs long-term observation and follow-up to conclude whether the incidence of rod fracture and pseudarthrosis can be reduced.
5. Case presentation
5.1 Case one
It was a 69-year-old female who complained of low back pain for 7 months, aggravated with weakness and pain in the right leg for 1 month. She was diagnosed with T12 and L5 multiple myeloma. Preoperative examinations showed L5 vertebral destruction and the spinal canal compression (white arrow). The L5 vertebrae were resected trans-right-pedicle and T12 was augmented with cement. The lumbar spine was fixed from L3 to S1. The multiple trajectory anchoring (MTA) technique was applied bilaterally to strengthen the internal fixation, which made it possible to avoid fixing the pelvis and made the surgery less invasive. Postoperative computed tomography (CT) scan showed the trajectory of pedicle screw (PS), cortical bone trajectory (CBT) screws, and sacral alar screws (Figure 2).
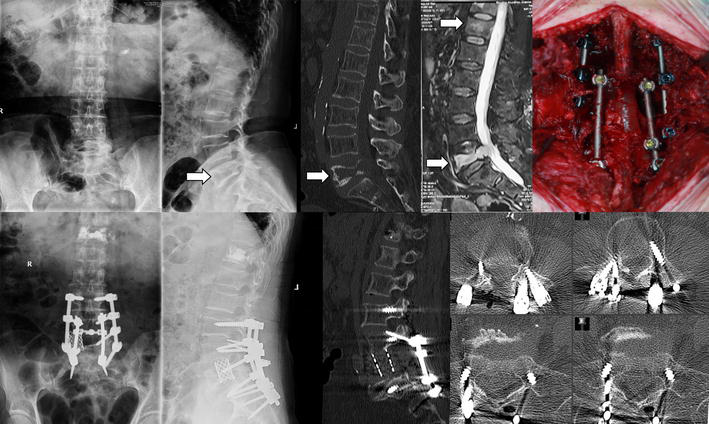
Figure 2.
The application of multiple trajectory anchoring (MTA) technique in the L5 vertebrae resection case.
5.2 Case two
It was a 51-year-old male patient who had severe back pain and radiating right leg pain for 30 years and was diagnosed with congenital scoliosis and lumbar spinal stenosis at L4/5. The scoliosis was generated by the L5 hemivertebrae on the right side (white arrow). L5 hemivertebrae resection and L2 to S1 fusion was performed posteriorly. The multiple trajectory anchoring (MTA) technique was applied to enhance the distraction force on the concave side and strengthen the internal fixation (Green arrow shows the CBT screw and yellow arrow shows the sacral alar screw). The postoperative images showed that the deformity was corrected well with a short-segment operation without fixing down to the pelvis (Figure 3).
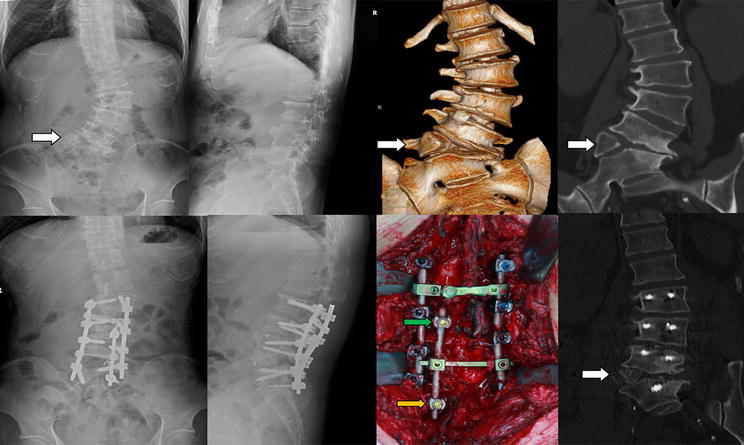
Figure 3.
The application of multiple trajectory anchoring (MTA) technique in the L5 hemivertebrae resection case.
5.3 Case three
It was a 69-year-old male patient with multi-level lumbar spinal stenosis from L3 to S1. Posterior lumbar decompression and interbody fusion from L3 to S1 was performed. During the surgery, the left pedicle of L5 was fractured due to excessive spinal decompression. In such case, the multiple trajectory anchoring (MTA) technique could be applied by inserting the L4 cortical bone trajectory (CBT) screw and sacral alar screw to enhance the pedicle screw (PS) internal fixation (Green arrow shows the CBT screw and yellow arrow shows the sacral alar screw) (Figure 4).
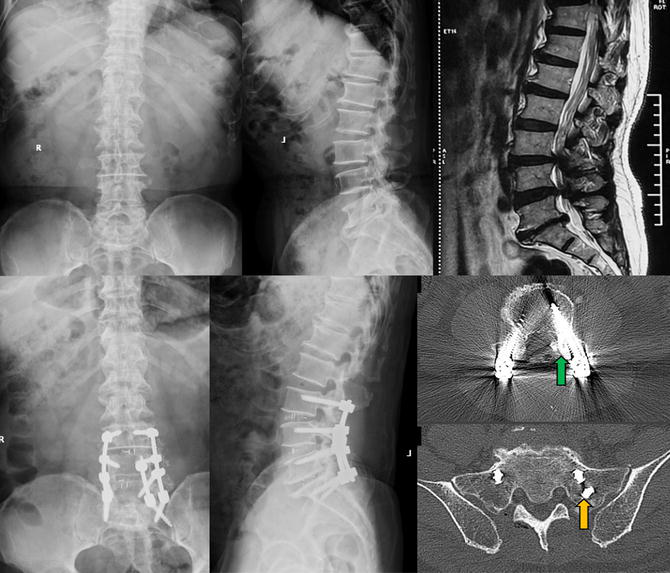
Figure 4.
The application of multiple trajectory anchoring (MTA) technique to reinforce the pedicle screw construction.
5.4 Case four
It was a 70-year-old male who had severe back pain and left leg pain for 4 months. He was diagnosed with L4 burst fracture and osteoporosis (T score of the bone mineral density was −5.0 in lumbar spine). Posterior L4 corpectomy and L2 to S1 fixation with bone cement augmentation was performed. To prevent internal fixation from loosening, additional fixation was performed using the MTA technique, in which left CBT screw and sacral alar screw were inserted and linked with the rod and connector (Green arrow shows the CBT screw and yellow arrow shows the sacral alar screw) (Figure 5).
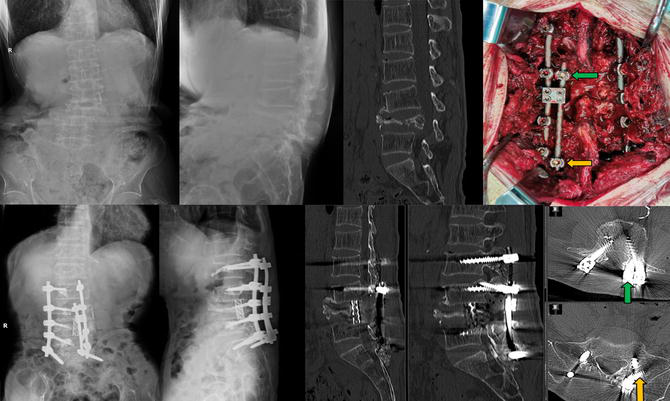
Figure 5.
The application of multiple trajectory anchoring (MTA) technique in the L4 vertebrae resection and severe osteoporotic case.
References
- 1.
Katz JN, Harris MB. Lumbar spinal stenosis. New England Journal of Medicine. 2008; 358 (8):818-825 - 2.
Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. 2016; 352 :h6234 - 3.
Suk S-I et al. Pedicle screw instrumentation in adolescent idiopathic scoliosis (AIS). European Spine Journal. 2012; 21 :13-22 - 4.
Umeta RS, Avanzi O. Techniques of lumbar-sacral spine fusion in spondylosis: Systematic literature review and meta-analysis of randomized clinical trials. The Spine Journal. 2011; 11 (7):668-676 - 5.
Wu A-M et al. Lumbar spinal stenosis: An update on the epidemiology, diagnosis and treatment. AME Medical Journal. 2017; 2 - 6.
Santoni BG et al. Cortical bone trajectory for lumbar pedicle screws. The Spine Journal. 2009; 9 (5):366-373 - 7.
Ueno M et al. Posterior corrective fusion using a double-trajectory technique (cortical bone trajectory combined with traditional trajectory) for degenerative lumbar scoliosis with osteoporosis. Journal of Neurosurgery: Spine. 2013; 19 (5):600-607 - 8.
Matsukawa K et al. In vivo analysis of insertional torque during pedicle screwing using cortical bone trajectory technique. Spine (Phila Pa 1976). 2014; 39 (4):E240-E245 - 9.
Li HM et al. Biomechanical fixation properties of the cortical bone trajectory in the osteoporotic lumbar spine. World Neurosurgery. 2018; 119 :e717-e727 - 10.
Wu X et al. A finite-element analysis on biomechanical performance of lumbar cortical bone trajectory versus traditional trajectory screw fixation in osteoporosis. Orthopedic Journal of China. 2018; 26 (12):1126-1131 - 11.
Hegazy AA, Hegazy RA. Midsagittal anatomy of lumbar lordosis in adult egyptians: MRI study. Anatomy Research International. 2014; 2014 :370852 - 12.
Sebaaly A et al. Etiology, evaluation, and treatment of failed Back surgery syndrome. Asian Spine Journal. 2018; 12 (3):574-585 - 13.
Rodriguez A et al. Novel placement of cortical bone trajectory screws in previously instrumented pedicles for adjacent-segment lumbar disease using CT image-guided navigation. Neurosurgical Focus. 2014; 36 (3):E9 - 14.
Takata Y et al. Hybrid technique of cortical bone trajectory and pedicle screwing for minimally invasive spine reconstruction surgery: A technical note. The Journal of Medical Investigation. 2014; 61 (3-4):388-392 - 15.
Guevara-Villazón F et al. Multiple-rod constructs in adult spinal deformity surgery for pelvic-fixated long instrumentations: An integral matched cohort analysis. European Spine Journal. 2020; 29 (4):886-895 - 16.
Hyun SJ et al. Comparison of standard 2-rod constructs to multiple-rod constructs for fixation across 3-column spinal osteotomies. Spine (Phila Pa 1976). 2014; 39 (22):1899-1904 - 17.
Merrill RK et al. Multi-rod constructs can prevent rod breakage and Pseudarthrosis at the lumbosacral junction in adult spinal deformity. Global Spine Journal. 2017; 7 (6):514-520 - 18.
Yamato Y et al. Long additional rod constructs can reduce the incidence of rod fractures following 3-column osteotomy with pelvic fixation in short term. Spine Deformity. 2020; 8 (3):481-490 - 19.
Hallager DW et al. Use of supplemental short pre-contoured accessory rods and cobalt chrome alloy posterior rods reduces primary rod strain and range of motion across the pedicle subtraction osteotomy level: An In vitro biomechanical study. Spine (Phila Pa 1976). 2016; 41 (7):E388-E395 - 20.
La Barbera L et al. Biomechanical advantages of supplemental accessory and satellite rods with and without interbody cages implantation for the stabilization of pedicle subtraction osteotomy. European Spine Journal. 2018; 27 (9):2357-2366 - 21.
Seyed Vosoughi A et al. Optimal satellite rod constructs to mitigate rod failure following pedicle subtraction osteotomy (PSO): A finite element study. The Spine Journal. 2019; 19 (5):931-941 - 22.
Echt M et al. A systematic review of treatment strategies for the prevention of junctional complications after long-segment fusions in the osteoporotic spine. Global Spine Journal. 2021; 11 (5):792-801 - 23.
Myung KS, Lee C, Skaggs DL. Early pelvic fixation failure in neuromuscular scoliosis. Journal of Pediatric Orthopedics. 2015; 35 (3):258-265 - 24.
Shabtai L et al. Sacral alar iliac (SAI) screws fail 75% less frequently than iliac screws in neuromuscular scoliosis. Journal of Pediatric Orthopedics. 2017; 37 (8):e470-e475 - 25.
Luca A et al. Instrumentation failure following pedicle subtraction osteotomy: The role of rod material, diameter, and multi-rod constructs. European Spine Journal. 2017; 26 (3):764-770 - 26.
Diebo BG et al. Adult spinal deformity. Lancet. 2019; 394 (10193):160-172 - 27.
DeWald CJ, Stanley T. Instrumentation-related complications of multilevel fusions for adult spinal deformity patients over age 65: Surgical considerations and treatment options in patients with poor bone quality. Spine (Phila Pa 1976). 2006; 31 (19 Suppl):S144-S151 - 28.
Lee CK et al. Influence of osteoporosis following spine surgery on reoperation, readmission, and economic costs: An 8-year Nationwide population-based study in Korea. World Neurosurgery. 2021; 149 :e360-e368 - 29.
Matsukawa K et al. Biomechanical evaluation of cross trajectory technique for pedicle screw insertion: Combined use of traditional trajectory and cortical bone trajectory. Orthopaedic Surgery. 2015; 7 (4):317-323 - 30.
Sansur CA et al. Biomechanical fixation properties of cortical versus transpedicular screws in the osteoporotic lumbar spine: An in vitro human cadaveric model. Journal of Neurosurgery. Spine. 2016; 25 (4):467-476 - 31.
Ueno M et al. Posterior corrective fusion using a double-trajectory technique (cortical bone trajectory combined with traditional trajectory) for degenerative lumbar scoliosis with osteoporosis: Technical note. Journal of Neurosurgery. Spine. 2013; 19 (5):600-607 - 32.
Huiqiang H et al. Cortical bone trajectory and traditional trajectory combined with satellite rod fixation for degenerative scoliosis. Chinese Journal of Spine and Spinal Cord. 2020; 30 (01):8-12 - 33.
Jain A et al. Pelvic fixation in adult and pediatric spine surgery: Historical perspective, indications, and techniques: AAOS exhibit selection. JBJS. 2015; 97 (18):1521-1528 - 34.
Shen FH et al. Pelvic fixation for adult scoliosis. European Spine Journal. 2013; 22 :265-275 - 35.
Kim YJ et al. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: Prevalence and risk factor analysis of 144 cases. Spine (Phila Pa 1976). 2006; 31 (20):2329-2336 - 36.
Weistroffer JK et al. Complications in long fusions to the sacrum for adult scoliosis: Minimum five-year analysis of fifty patients. Spine (Phila Pa 1976). 2008; 33 (13):1478-1483 - 37.
De la Garza Ramos R et al. Iliac screw versus S2 alar-iliac screw fixation in adults: A meta-analysis. Journal of Neurosurgery. Spine. 2018; 30 (2):253-258 - 38.
Keorochana G et al. Comparison of complications and revisions after sacral 2 alar iliac screw and iliac screw fixation for Sacropelvic fixation in pediatric and adult populations: Systematic review and meta-analysis. World Neurosurgery. 2019; 132 :408-420.e1 - 39.
Ilyas H, Place H, Puryear A. A comparison of early clinical and radiographic complications of iliac screw fixation versus S2 alar iliac (S2AI) fixation in the adult and pediatric populations. Journal of Spinal Disorders & Techniques. 2015; 28 (4):E199-E205 - 40.
Hasan MY et al. Postoperative complications of S2AI versus iliac screw in spinopelvic fixation: A meta-analysis and recent trends review. The Spine Journal. 2020; 20 (6):964-972