Abstract
Multilevel spine degeneration with deformity should be described in 3 column theory of lumbar degeneration cascade to detect completely the degenerative damages or deformers. Theory of degenerative spine deformity is a combination between 2 factors: 1. spine stabilizer (disc, 2 facet joints, anterior and posterior longitudinal ligament, supraspinatus ligament, multifidus muscle) and 2. spine deformer (degenerative injury). The common gold standard is to remove the deformer by open surgery, but this open surgery will sacrifice the stabilizer, so it requires artificial stabilizer or fusion device. The concept of minimally invasive endoscopic spine surgery is simply to remove the deformer while retaining the stabilizer. After deformer are removed, the stabilizers will be reapplied, and the deformity can be corrected naturally.
Keywords
- endoscopy
- spine degeneration
- deformity
- fusion
- 3 column theory
1. Introduction
Surgery for treatment of multilevel spine degeneration with deformity, where are we now: open surgery, minimally invasive spine surgery, fusion or non-fusion. In fusion technique related to the nature of illness, the degenerative cascade will go to the adjacent level [1, 2, 3, 4, 5, 6, 7]. In non-fusion technique or decompression, the degenerative damages should be removed completely related to the nature of illness [8, 9, 10].
The theory of nature of illness in spine degeneration and deformity, including the nature of healing after surgery, will be discussed.
2. Three columns theory of lumbar degenerative
2.1 Cascade and classification
The axial stability is maintained along a vertical column system, three columns from C2 to the sacrum. The anterior column is formed by the vertebral bodies and discs, and the two posterior columns by posterior joints. Anterior column consist of vertebral bodies, discs, anterior, and posterior ligament. The articular facet joint and flavum ligament are middle column, while the posterior column consist of spinous process, inter- and supraspinatus ligament include multifidus muscle [11, 12, 13, 14].
Three joint complex theory of lumbar degenerative cascade by Kirkaldy-Willis et al. described the detail of pathologic changes of the disc and two posterior joints, but this only describe the 2 vertical columns, anterior and middle column [15]. Christian Ingerslev Baastrup a Danish radiologist Copenhagen [16] described degenerative cascade of the posterior vertical column, pathologic changes on the spinous processes in the lumbar vertebrae including the soft tissues between them which was mentioned as kissing spine. His publication was supported by studies by Auckland and Bristol study group (2010), described a breakdown of the inter-spinous ligament and leading to a development of neo-arthrosis between adjacent spinous processes, characterized by abutment, enlargement, sclerosis and bursa [12, 14, 16, 17, 18].
The new three columns theory of Lumbar degenerative cascade related to the nature of illness of lumbar degeneration is built combining both theory to give a clear understanding about lumbar degenerative process: that may start from either one of the three columns, alone or together, starting from inflammatory to a compressive reactions, change the bio-mechanic construct of the lumbar spine, single or multi-levels and leading to a deformity or de novo scoliosis (Figure 1) [12, 14].

Figure 1.
De novo scoliosis.
The new classification based on three columns theory of lumbar degenerative cascade could give a complete description about the various individual cascade of lumbar degeneration, and has the consequence in the clinical application of evidence-based treatment related to this theory: the justification of treatment for various individual cases will be different. The classification should describe a complete assessment of the bio-mechanic construct changes due to degenerative damages involving the three columns using the radiologic parameters of dynamic lumbosacral x-rays and MRI studies and could show the different cascade of each column. The grading classification consist of:
Grade 1, involve either one of the columns, each level in different cascade,
Grade 2, involve either 2 columns, each column or level in different cascade,
Grade3, involve 3 columns, each column or level in different cascade (Figure 2).
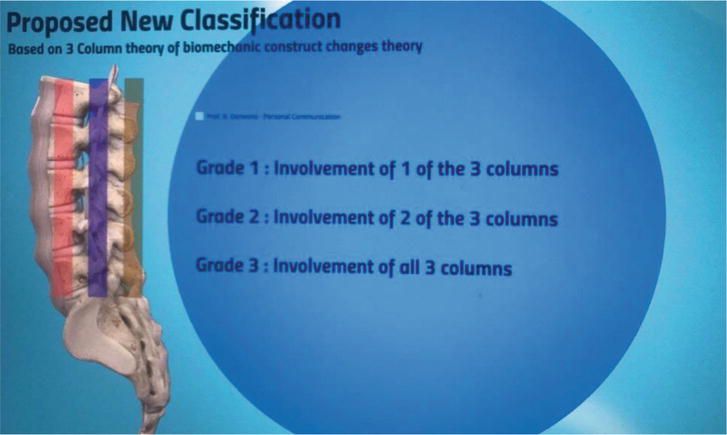
Figure 2.
Proposed new classification.
Purpose of this classification is to describe completely the bio-mechanic construct changes due to degenerative damages, involving all column of mobile segment, each column in different level and different cascade. It can be used as a guideline to fix and reconstruct all the degenerative damages, specially in preserving the spine motion, as an evidence-based consideration to justify the different methods of treatment for the various cases of lumbar degeneration [14].
3. Degenerative spine deformity
Lumbar spine stability during the dynamic movement is supported by disc, facet joint and strong ligament: anterior longitudinal, posterior longitudinal, and supraspinatus ligament complex. According to Wolfgang Rauschning the supraspinatus ligament complex is not a ligament, but multiple tendon insertion of multifidus muscle [10, 13, 14, 19, 20, 21, 22, 23, 24, 25]. All the above anatomy including the muscle are known as spine stabilizer (Figure 3).
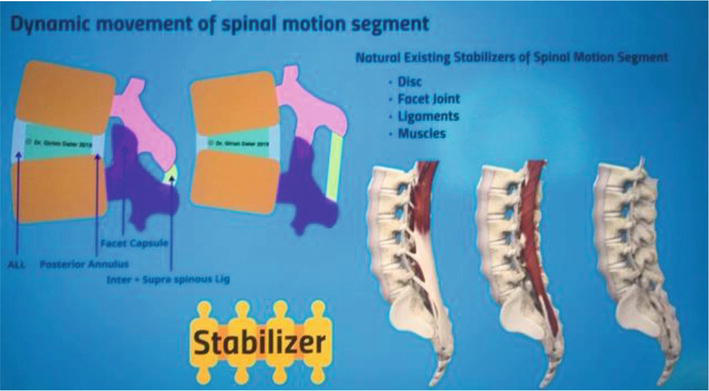
Figure 3.
Spine stabilizer.
Anatomical changes due to degenerative damage occur in three columns: osteophyte, hypertrophy facet, lamina, spinous process, canal stenosis, disc herniation, disc narrowing, flavum in-folding and hypertrophy, kissing spine, kissing lamina, all of these are known as deformer in degenerative cascade because it will dysfunction the spine stabilizer (Figure 4) [14].
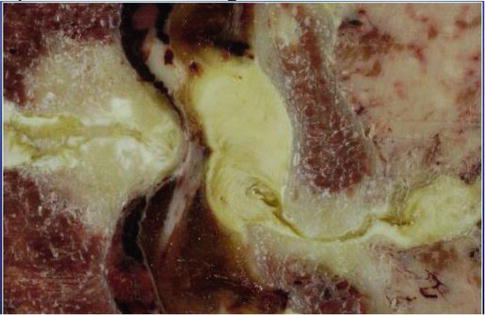
Figure 4.
Kissing lamina as deformer (courtesy of Rauschning).
The degenerative spine deformity is a combination between two factors: spine stabilizer and spine deformer, creating instability and deformity in the three columns (Figure 5).

Figure 5.
Deformity as combination of two factors.
4. Option of treatment
The gold standard of treatment is open surgery or decompression to remove the deformer, but anyway this technique will sacrifice some of the stabilizer and as a consequence need to use artificial stabilizer or fusion to restabilize (Figure 6) [19, 20, 26, 27].
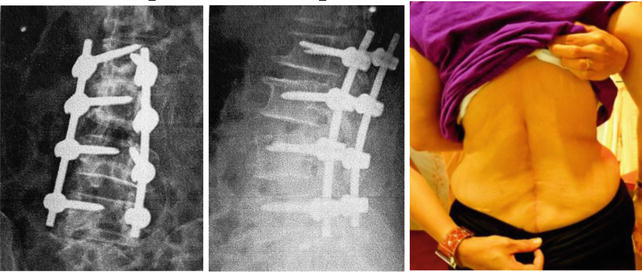
Figure 6.
Artificial stabilizer.
The question is, if the technique of surgery could preserve the stabilizer, does the artificial stabilizer is needed. Minimally invasive spine surgery using endoscope was developed to answer the question. A long evolution in developing this technology starting from Hijikata 1970s, Parviz Kambin 1980s, Screiber, Suezawa, Leu using discoscopy late 1980, Anthony Yeung transforaminal under continuous irrigation 1990s, Sebastian Rutten interlaminar and application of arthroscopic technique 2000s.
The disruptive surgical technology of spine endoscope is from dry environment in simple endoscopy to arthroscopic surgical dissection performed in the spine underwater with continuous irrigation and suction. Advantages of disruptive technology are:
docking system and closed system irrigation, the water irrigation and suction could be controlled better,
the continuous water irrigation will create a better visibility in the surgical area, reduce intra and postop bleeding and infection rate significantly,
the range of approaches increased from pure transforaminal or posterolateral to interlaminar, because rongeur, high-speed drills, other instruments could be used and has a wider horizon of view.
The current indication spectrum for lumbar, thoracic, and cervical applications become wide and covers all types of degenerative (and other) pathologies, which have been the domain of microsurgical techniques in the past.
The new concept of endoscopic surgical technique based on three columns theory is:
Preserve the three columns spine stabilizers.
Decompression to remove spine de-formators due to degenerative damage constricting the spinal canal in three columns.
Decompression will naturally refunction the spine stabilizers and could reduce the deformity without using artificial stabilizers.
Deformity reduction is similar as the second decompression, because the best decompression is deformity correction.
5. Cases
Case 1: Lady 83, Low back pain and sciatica, spine deformity, wheelchair case. MRI show lumbar spondylosis with severe stenosis on L 3-4 and L 4-5. Treatment by endoscopic decompression from interlaminar and deformity was corrected well (Figures 7 and 8).
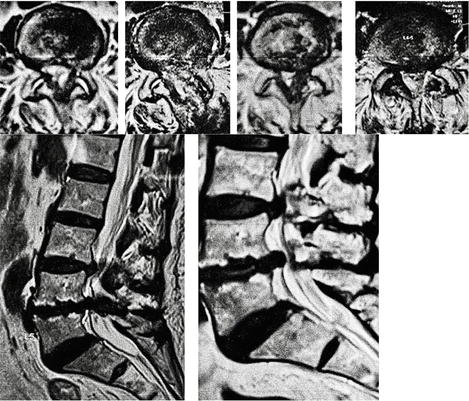
Figure 7.
MRI L 3-4, L 4-5, before and after endoscopic treatment.
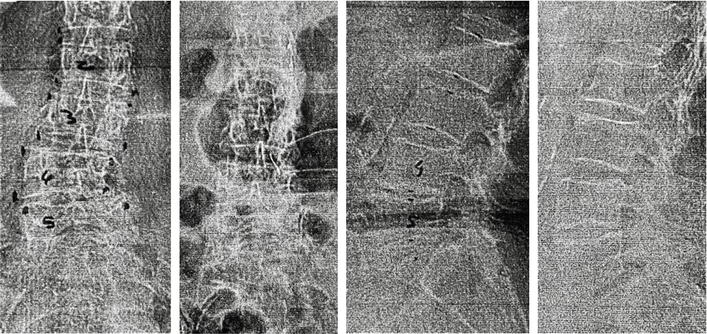
Figure 8.
Deformity corrected.
Case 2: Lady 62, Low back pain and sciatica with deformity, on MRI lumbar spondylosis L 2-3, 3-4, 4-5. Deformity was corrected after decompression by endoscopic interlaminar (Figures 9 and 10).

Figure 9.
MRI L2-3, 3-4, 4-5 before and after surgery.
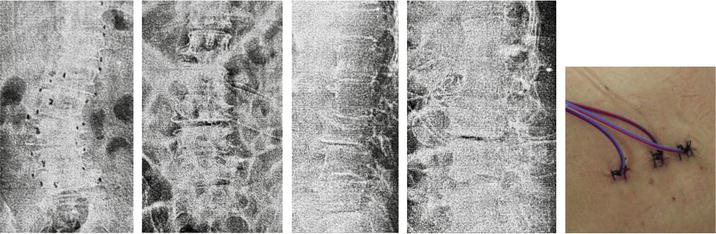
Figure 10.
Deformity corrected.
Case 3: Lady 55, low back pain and sciatica with deformity, claudication, wheelchair case. On MRI lumbar spondylosis and severe stenosis L 4-5. Deformity correction after endoscopic decompression interlaminar (Figures 11 and 12).
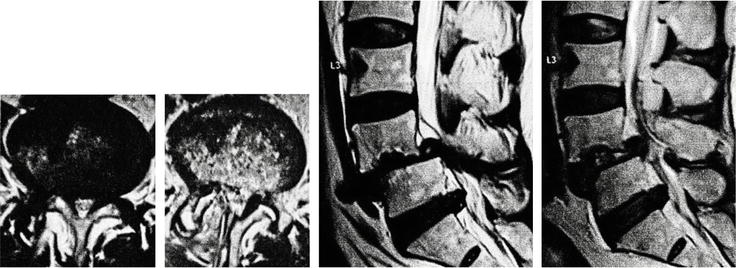
Figure 11.
MRI before and after surgery L 4-5.
Figure 12.
Deformity corrected.
6. Conclusion
Spine is a life tissue and has the nature of healing after surgery that should be well supported. The new classification of spine degeneration describe all deformer of spine degeneration in three columns. Degenerative spine deformity is a combination of 2 factors: spine stabilizer and deformer. Removing all deformer could support the function of spine stabilizer to reduce the deformity. The disruptive technology of endoscopy using arthroscopic concept for the spine could remove all deformer while retaining the spine stabilizer. After deformer is removed, the stabilizer will be reapplied and the deformity can be corrected naturally.
References
- 1.
Eck JC, Humphreys SC, Hodges SD. Adjacent-segment degeneration after lumbar fusion. A review of clinical, biochemical, and radiologic studies. The American Journal of Orthopedics. 1999; 28 :336-340 - 2.
Etebar S, Cahill DW. Risk factors for adjacent-segment failure following lumbar fixation with rigid instrumentation for degenerative instability. Journal of Neurosurgery. 1999; 90 :163-169 - 3.
Lee CK. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine. 1988; 13 (3):375-377 - 4.
Lindsey DP, Swanson KE, Fuchs P, et al. The effects of an interspinous implant on the kinematics of the instrumental and adjacent levels in the lumbar spine. Spine. 2003; 28 (19):2192-2197 - 5.
Molz F, Partin J, Kirkpatrick J. The acute effect of L3/L4 fusion on the motion of vertebrae in whole lumbar cadaveric spine. In: Presented at the Annual Meeting of the International Society for the Study of the Lumbar Spine; Vancouver, BC. 2003 - 6.
Patel C, Truumees E, Gittlin J, et al. Symptomatic spinal stenosis adjacent to a previous lumbar fusion. The Spine Journal. 2002; 2 :54S-55S - 7.
Weinhoffer SL, Guyer RD, Herbert M, et al. Intradiscal pressure measurements above an instrumented fusion. A cadaver study. Spine. 1995; 20 (5):526-531 - 8.
Kanayama M, Hashimoto T, Shigenubu K, et al. Adjacent-segment morbidity after graft ligamentoplasty compared with posterolateral lumbar fusion. Journal of Neurosurgery. 2001; 95 (1 Suppl):5-10 - 9.
Kanayama M, Hashimoto T, Shigenubu K, et al. Non-fusion surgery for degenerative spondylolisthesis using artificial ligament stabilization: Surgical indication and clinical results. Spine. 2005; 30 (5):588-592 - 10.
Stoll TM, Dubois G, Schwarzenbach O. The dynamic neutralization system for the spine: A multi-center study of a novel non-fusion system. European Spine Journal. 2002; 11 (Suppl. 2):170-178 - 11.
Roy-Camille R. Traitement des fractures du rachis dorsolumbaire par la method de Bohler. Revue de Chirurgie Orthopédique et Réparatrice de l'Appareil Moteur. 1989; 75 (7):E109-E114 - 12.
Darwono B, Radchenko V. New classification 3 columns theory of lumbar degenerative cascade (literature review). Orthopaedics, Traumatology and Prosthetics. 2018; 610 (1):96-104. DOI: 10.15674/0030-59872018196-104 - 13.
Louis R. Spinal stability as defined by the three-column spine concept. Anatomica Clinica. 1985; 7 :33-42 - 14.
Darwono B. MISS Concept based on theory of three columns-lumbae degenerative cascade. In: Bambang Darwono: Presented at SICOT 42th Annual Meeting, Kuala Lumpur, Malaysia. 2022 - 15.
Kirkaldy-Willis WH, Wedge JH, Yong-Hing K, et al. Pathology and pathogenesis of lumbar spondylosis and stenosis. Spine. 1978; 3 :319-328 - 16.
Baastrup C. On the spinous processes of the lumbar vertebrae and the soft tissue between them, and on pathological changes in that region. Acta Radiologica. 1933; 14 :52-54 - 17.
Aylott CE, Puna R, Robertson PA, Walker C. Spinous process morphology: The effect of ageing through adulthood on spinous process size and relationship to sagittal alignment. European Spine Journal. 2012; 21 (5):1007-1012. DOI: 10.1007/s00586-011-2029-6 - 18.
Kwong Y, Rao N, Latief K. MDCT findings in Baastrup disease: Disease or normal features of the aging spine? AJR. American Journal of Roentgenology. 2011; 196 (5):1156-1159. DOI: 10.2214/AJR.10.5719 - 19.
Frymoyer JW, Krag MH. Spinal stability and instability: Definitions, classification, and general principles of management. In: Kahn A, editor. The Unstable Spine. New York: Grune & Startton; 1986 - 20.
Frymoyer JW, Sellby DK. Segmental instability. Rationale for treatment. Spine. 1985; 10 :280-286 - 21.
Fujiwara A, Lim TH, An HS, et al. The effect of disc degeneration and facet joint osteoarthritis on segmental flexibility of the lumbar spine. Spine. 2000; 25 (23):3036-3044 - 22.
Fujiwara A, Tamai K, An HS, et al. The relationship between disc degeneration, facet joint osteoarthritis, and stability of the degenerative lumbar spine. Journal of Spinal Disorders. 2000; 13 :444-450 - 23.
Okawa A, Shinomiya K, Komori H, et al. Dynamic motion study of the whole lumbar spine by video-fluoroscopy. Spine. 1998; 23 (916):1743-1749 - 24.
Paajanen H, Tertti M. Association of incipient disc degeneration and instability in spondylolisthesis. A magnetic resonance and flexion-extension radiographic study of 20-year-old low back pain patients. Archives of Orthopaedic and Trauma Surgery. 1991; 111 :16-19 - 25.
Pearcy MD, Tibrewal SB. Lumbar intervertebral disc and ligament deformations measured in vivo. Clinical Orthopaedics; 184, 191 :281-286 - 26.
DePalma AF, Rothman RH. Surgery of the lumbar spine. Clinical Orthopaedics. 1969; 63 :162-170 - 27.
Keller TS, Hanson TH, Abram AC, et al. Regional variations in the compressive properties of lumbar vertebral trabeculae. Effect of disc degeneration. Spine. 1989; 14 :1012-1019