Abstract
Interspinous devices (or spacers) are currently used in lumbar spine surgery, but their use is still controversial, mainly due to confusion between so-called first and second-generation spacers, and unrespect of formal indications to implant. Our first aim is trying to offer an interpretation for a correct indication of surgical implantation, paying additional attention to those pathological conditions in which these devices must not be used; second, to identify the right clinico-surgical method to avoid potential errors in this surgery; third, to stress those surgical tricks directed to perform a successful implant of these spacers.
Keywords
- interspinous device
- interspinous spacer
- lumbar spine stenosis
- lumbar spine surgery
- neurogenic intermittent claudication
1. Introduction
Nowadays, surgical implantation of lumbar interspinous devices (ISDs) has a widely accepted role in the management of spinal degenerative disorders, and this is confirmed by the current high number of scientific papers dealing with their use. Nevertheless, the issue of ISDs still remains quite controversial, and this is mainly due to two reasons: first, experimental data are often misinterpreted and therefore not considered strong enough to justify a clinical application; second, sometimes, indication to an ISD implant isn’t done in a correct way and the subsequent potential poor surgical outcome being then attributed to the ISD itself (and not to the surgeon!); third, the technique of implantation of an ISD is too often deemed ‘easy’ and, hence, those basic surgical steps not respected, so opening the way to poor postoperative results.
2. Historical remarks
We are indebted to Prof. Jacques Sénégas, who first elaborated the concept of ‘lumbar dynamic fixation’ about forty years ago and developed the ISD named Wallis [1]. Since then, a deluge of ISDs, often having different experimental and clinical supports, have been marketed and scientific papers concerning their use go on to be published; this context led to an unfavourable confusion about their correct use and, of course, careful and free from prejudices evaluation of clinical application and outcome.
3. Experimental data
Biomechanical studies have shown that all of ISDs act grossly in the same way: they enlarge spinal canal dimensions, increase neuro-foramina height, reduce intradiscal pressure in neutral and extended position [2]; moreover, they have a ‘primary stabilizing effect’ [3]. The ISDs designed ‘for fusion’ additionally show to promote bone fusion at the instrumented level.
4. Interspinous devices
ISDs may be grouped into two categories: the first group includes the so-called ‘simple’ spacers (first-generation), and the second one is constituted by the spacers ‘for fusion’ (second-generation); ‘simple’ spacers maybe static or dynamic (the term ‘elastic’ is sometimes used to indicate some dynamic devices). We’ll here take in consideration some of the most frequently implanted (and studied) devices, remembering that some of them are no more marketed.
4.1 Spacers ‘simple’

Figure 1.
Lumbar stenosis. Sagittal CT scan at 15-year follow-up: the Wallis spacers, correctly placed, are visualized at L3-L4 and L4-L5 (
4.2 X-STOP (taken off the market)
4.3 Spacers ‘for fusion’

Figure 2.
Thoracic degenerative disc disease. Lateral x-ray film: the ASPEN device is correctly inserted at the mid-thoracic indexed level.

Figure 3.
Thoracic degenerative disc disease. Lateral x-ray film: the SEASPINE device is well visualized at the mid-thoracic indexed level.

Figure 4.
Spacers ‘for fusion’. Sagittal MR T1-weighted image at 2-year follow-up: the BACFUSE spacer is seen at L4-L5 (
5. Indications
Main indications for an ISD implant are grouped under the wide term of lumbar spine degenerative disorder; although this comprehensive definition may represent a protective shield for the surgeon, we strongly recommend trying to obtain an exact preoperative diagnosis, not only because ‘the more correct the indication, the higher the rate of success of the intervention’, but also because, concerning the term of lumbar degenerative conditions, instructions for use (IFUs) of different ISDs may vary. Therefore, we’ll here describe different degenerative lumbar disorders amenable to ISD implants.
5.1 Central stenosis
Central lumbar canal stenosis probably represents the most important indication of an ISD implant, and this has been extensively confirmed. Having this said, the main relevant aspects are two: performing or not decompression of neural structures before ISD implant, and coexistence of a listhesis which could be not adequately treated by ISD. About the first point, the decision to perform a decompressive step may be taken simply based on preoperative magnetic resonance (MR) or computed tomography (CT) scans and this is unequivocally true for severe stenosis causing bilateral NIC (Figure 5). Milder degrees of central stenosis could not necessarily require pre-ISD neural decompression; in such an occurrence, intraoperatively we behave as follows: after having skeletonized the indexed level, the application of traction on spinous processes (using two Backhaus forceps) is made; if frank hypermobility is appreciated, the ISD is inserted without delivering a flavo-laminotomy, because we know that it will realize an enlargement of the central canal and restore the bi-foraminal height, such to obtain a sufficient neural decompression (as we say, ‘
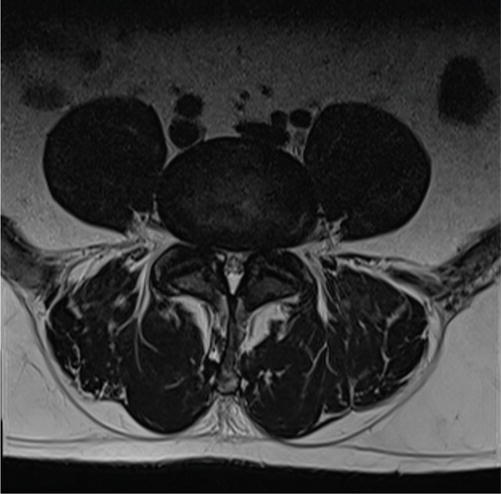
Figure 5.
Severe lumbar central stenosis. Axial MR T2-weighted image: preoperative study.
5.2 Foraminal stenosis
This is probably one of the most correct and valuable indications (Figure 6). Intraoperatively, after having performed a plain microsurgical foraminotomy on the affected side, only minimal contralateral skeletonization will be necessary before applying the ISD. We here must remember that in these cases, the choice of the ISD could favour those spacers, which can be inserted by sparing the supraspinous ligament.
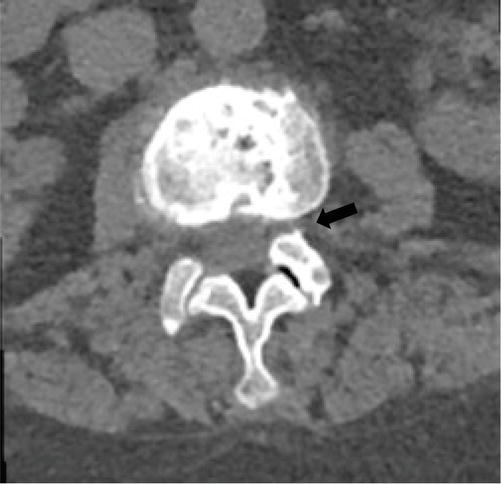
Figure 6.
Lumbar foraminal stenosis. A preoperative axial CT scan shows the marked narrowing of the left neuroforamen (
5.3 Recurrent disc herniation
Operated lumbar disc herniations may recur in different ways; clinical presentation is often persistent back pain, exacerbated by movements, associated with radicular irradiation, and the MR scan may show a small extruded disc fragment, surrounded by scar tissue, just at the entry of the neuroforamen; such condition, usually refractory to medical and physical therapy, is the ideal target for a micro-surgical decompression of the involved nerve root(s), associated with a selective discectomy, followed by ISD implant.
5.4 Isolated disc herniation
Implantation of an ISD has no role in treating an isolated primary lumbar disc herniation; however, some empirical evidence delineates a long-term reduced rate of recurrent disc herniation when a spacer is applied at the end of the removal of the extruded disc. In those selected cases in which the herniated fragment is associated with a frank degenerated disc, causing intense low-back pain, the option of the additional insertion of an ISD may be considered [12].
5.5 DDD
As already stated in Section 3, ISDs reduce intradiscal pressure and have a stabilizing effect [which is quantitatively comparable to ALIF, meaning about 50% reduction of range of motion (ROM)]; basing upon these experimental data, we implanted ISD in several cases of single DDD, obtaining good results in terms of long-lasting back pain relief (Figure 7). We wish to stress the occurrence of a hyperintense signal of interspinous ligament in MR T2-weighted images, which must be considered an additional element of disc disease, hence supporting the indication of an ISD implant (Figure 8).

Figure 7.
Lumbar DDD. Sagittal MR T1-weighted scan at 6-year follow-up: the L5-S1 degenerated disc is well seen, and the spacer is correctly inserted between the two spinous processes (

Figure 8.
Lumbar degenerative disc disease (DDD). Preoperative sagittal MR T2-weighted image: the L5-S1 degenerative disc is shown, as well the hyperintense signal of the interspinous ligament (
5.6 Post-surgical instability
This is a well-known condition, which may follow one or more lumbar surgical procedures: refractory pain is mainly located at the low-back and flexion–extension x-ray films usually show minimal or no listhesis; these patients may be adequately treated by an ISD implant, which is safer than other invasive fixation procedures.
5.7 Spondylolisthesis
During a procedure aiming to stabilize a lumbar anterolisthesis, the matter of reducing the slipped vertebrae occurs, considering that reduction may potentially result in permanent nerve root damage; our experience led us to the conclusion that spinous fixation by means of a second-generation ISD plus additional bone fusion provides a valid result when used in those cases of spondylolisthesis up to grade-1 (Figure 9).

Figure 9.
Lumbar spondylolisthesis. Preoperative sagittal MR T2-weighted scan: the L4–L5 stenosis and listhesis grade-1 (
5.8 Synovial cyst
Lumbar synovial cysts are frequently diagnosed as the cause of lumbar and sciatic pain; except for rare instances of spontaneous resorption, most of these cysts require surgical removal; because of the association of satellite spondylolisthesis, which in our experience occurs in almost all cases, it may be advisable to correct the vertebral slippage contextually to the excision of the cyst. Associated anterolisthesis is never grade-2, so we routinely insert an ISD once the cyst is removed; our long-term follow-up x-ray controls demonstrate no need for additional stabilization procedures.
5.9 Transitional vertebra
Vertebral anomalies at the lumbosacral junction, named as sacralization of L5 or lumbarization of S1, are frequent and may give rise to refractory, mechanical back pain; in these cases, x-ray films usually show mild instability, which may appear as L5-S1 retrolisthesis. ISD implants proved to be effective in providing long-lasting, excellent back pain relief (Figure 10).

Figure 10.
Transitional vertebra. Preoperative sagittal MR T2-weighted scan: typical appearance of vertebral bodies and discs at the lumbosacral passage (
5.10 Adjacent segment disease
As already stated before (see Section 4), the implant of an ISD at the rostral level of a multilevel fixation may be useful to reduce the future risk of ASD. We never adopted this technique in a prophylactic way; however, we implant a second-generation ISD to treat those cases of ASD, in which a lumbar stenosis w/wo associated listhesis occurs rostrally or caudally to a previous posterior pedicular fixation (Figure 11). Of course, a careful evaluation of preoperative neuroradiological examination is mandatory to check the shape and volume of the spinous process to be included in the ISD anchor; intraoperatively, the terminal part of rods and the surgical scar may hinder skeletonization of the indexed spinous processes, but we never had to temporarily remove one of them to insert the ISD.
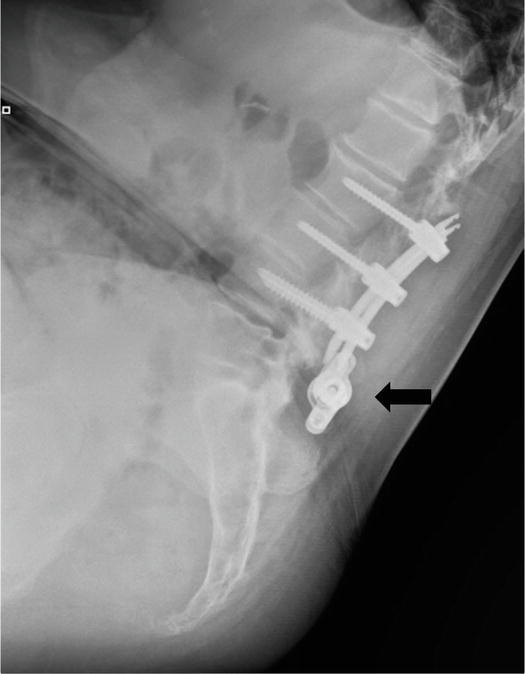
Figure 11.
Adjacent segment disease (ASD). Lateral x-ray film at 2-year post-ISD implant: pedicular fixation L2-L3-L4 is seen; the spacer at the caudal ASD level is well inserted between the spinous processes (
6. Contraindications
ISDs may differ from each other in several aspects; however, all of them share two important features: first, they cannot be implanted at the level of a pars defect; second, they cannot be used in case of a spondylolisthesis >grade-1.
Concerning the first occurrence, it must be stressed that sometimes preoperative neuroradiological exams may scotomize an isthmic defect and the related mild listhesis be wrongly attributed to a degenerative disorder; if so, intraoperatively, the surgeon will have to face an unexpected pathoanatomical finding and be obviously addressed to change surgical strategy timely.
Anterolisthesis grade-2 may involve different scenarios. A surgeon may incorrectly interpret preoperative images and judge a borderline slippage as grade I instead of grade II, often due to a misleading neuroradiological report; this is why a flexion–extension x-ray film is mandatory in the preoperative setup of a lumbar instability. Or, a frank listhesis, deemed by the experienced surgeon when unexpectedly found out at surgery, will discourage him from implanting the scheduled ISD and possibly shift to a pedicle fixation.
Of course, several additional disorders (such as osteoporosis, coexisting infective states, bone anomalies of the posterior vertebral arch, etc.) constitute a contraindication to the implant of an ISD, but they are easily ascertained at the time of preoperative consultation.
7. Surgical tricks
The interspinous space may present multiple anatomic variations, and this must be kept in mind by the surgeon, particularly the shape of the space and its matching with the shape of the spacer [13].
Regardless of the type of ISD, the basic rule to implant it successfully is to insert it as deep as possible, and the right placement is at the line of articular processes (Figure 12); suboptimal insertion of the spacer does not necessarily involve a poor clinical outcome, but x-ray follow-up controls, at least over the first postoperative year, are strongly recommended.
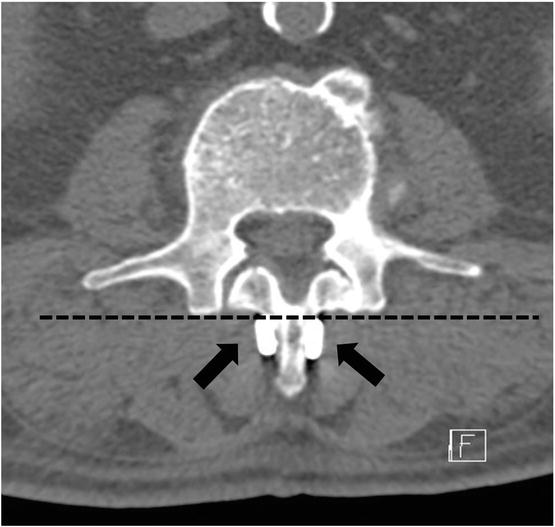
Figure 12.
Depth of ISD implant. Postoperative axial CT scan: the base of lateral plates of the spacer (
The surgical technique to implant an ISD may differ, and it’s also due to the type of spacer and the strumentarium to implant. Some spacers are to be applied through the interspinous ligament, assembling the two parts once they are
The last step of implantation is clamping the lateral plates of the spacer against spinous processes; this is probably the most hazardous manoeuvre in terms of risk of rupture of spinous process and must be done cautiously, squeezing the dedicated compressors in a step-by-step alternate way. Once you have compressed the device in situ, we suggest checking its final mechanical seal: the spacer is grabbed by a needle-holder and pulled superficially and horizontally, so observing that the lumbar segments move as a unique block.
Multilevel stenosis of the lumbar canal, though usually symptomatic at just one level, may be encountered in the daily practice and the matter of operate upon two or three levels is not trivial; are ISDs insertable at multiple levels? Yes, they are. However, much attention must be paid to the preoperative CT scan: the decisive factor is represented by the height of the middle of the three indexed spinous processes, which must be high enough to receive plates of both spacers (Figure 13). Based on our experience, the implant of two spacers having a metal-to-metal final construct at one or both sides of the middle spinous process may result in a poor clinical outcome in terms of back and/or radicular pain.

Figure 13.
Two-level lumbar spinal stenosis. Flexion x-ray film at 2-year follow-up: the spacers are correctly placed, and the construct is no metal-to-metal.
8. Complications
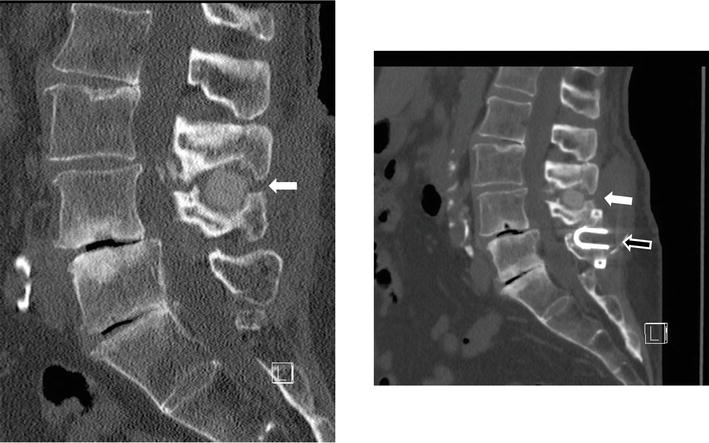
Figure 14.
‘Wrong level’. Sagittal reformatted CT scans: this patient came to our attention after having performed an “interspinous stabilization L4-L5” elsewhere (as reported in medical discharging chart); soon after surgery her bilateral
Regardless of the type of ISD used, most of the fractures involve the junction of the inner and middle thirds of the cranial spinous process. When we started inserting a PEEK ISD, the first bone fracture case was discovered only through CT scan, which we routinely performed on postoperative day 1, and it passed clinically unnoticed (
9. Personal considerations
Dutch school of neurosurgery goes on to keep a leading role in the management of spinal stenosis; over 70 years ago, in a tribute to another giant of spinal surgery (Clovis Vincent), Prof Verbiest first described the pathophysiological correlation between symptoms of cauda equina compression and spinal stenosis, which, curiously and interestingly, he defined as ‘rare’ [14]. Nowadays, the group of Moojen goes on sharing elegant works concerning the outcome of patients receiving an ISD implant: in their very recent randomized control trial paper, a 5-year follow-up good outcome in ISD implant, if compared to conventional lumbar decompression was reported [15]. Moreover, it’s worth that they also state that the ISD group seems to have less back pain during long-term follow-up; this constitutes a very important issue: our experience, using different types of ISD, supports the same conclusion: ISD patients, implanted for treating lumbar stenosis (and, above all, for a DDD), early in the postoperative course refer that back pain is of different quality and far milder than preoperatively, and this substantial pain relief maintains over time.
We started to implant ISDs in 2005, and since then, we have used different types of spacers; on time, we realized that each of them has its own pros and cons, which must be well-known by the surgeon to best adapt to any patient elected for this kind of surgery.
In my daily activity, patients affected by spondylolisthesis grade 2, in which implanting an ISD represents a formal contraindication, are very few; on the contrary, the number of cases harbouring a listhesis up to grade- 1 is far larger, and almost all of them are ideal candidates to ISD implant; this means that at least as first surgical management step, more invasive procedures (such as transpedicular fixation, anterior lumbar interbody fusion, XLIF, etc.) are not necessary.
Lumbar spinal stenosis affects about one-third of people aged 70, and those of them requiring a surgical treatment are offered different options, the first of whom being a decompressive one- or more-level laminectomy. Based upon our 30-year experience, we think that: a] standard one- or multilevel laminectomy [
Most of the scientific papers dealing with the outcome of different surgical operations, performed to achieve lumbar stabilization take bone fusion rate into account as the main indicator of success. This methodological approach was developed and consolidated more than 50 years ago when global aspects concerning this kind of surgery were different: hardware, age of patients (usually less than 80 years), and diagnostic tools (grossly limited to x-ray films). Nowadays, we feel that the concept of bone fusion, adopted to evaluate the outcome of surgical options for DDD and lumbar stenosis, should be replaced by that of ‘bone synthesis’, which is more helpful and adherent to global (functional, clinical, and radiological) analysis of operated patients.
One of most frequent criticisms made to ISDs is the absence of long-term follow-up studies; this may be partially true and it’s also due to the replacement of the first-generation spacers with the newest ones, probably making ongoing studies obsolete and, therefore, abandoned. Moreover, recent covid-19 epidemics determined a tremendous gap in the follow-up studies, especially concerning many aged patients operated upon for lumbar stenosis, who deceased or were lost over last three years. Currently, our documented experience with hundreds of implanted ISDs allows us to affirm that: (a) a first-generation PEEK spacer demonstrates no neuroradiological migration or bone spinous process rupture at a 13-year follow-up (Figure 15); (b) a second-generation device shows the same good result at a 10-year follow-up (Figure 16).
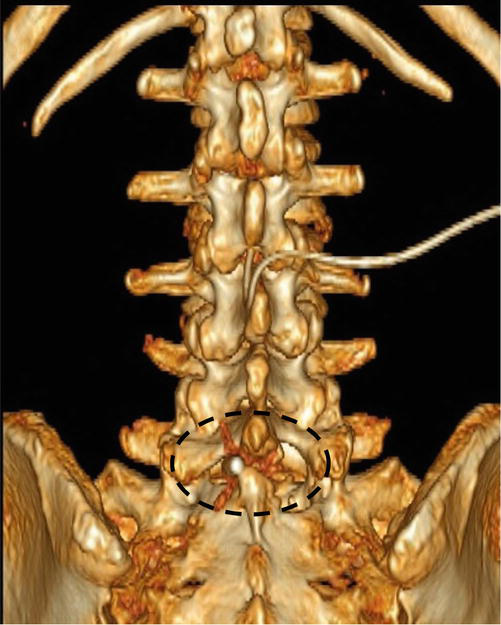
Figure 15.
Lumbar DDD. Three-dimensional reformatted coronal CT scan at 13-year follow-up: the BACJAC spacer is well inserted between the spinous processes of L5 and S1 (
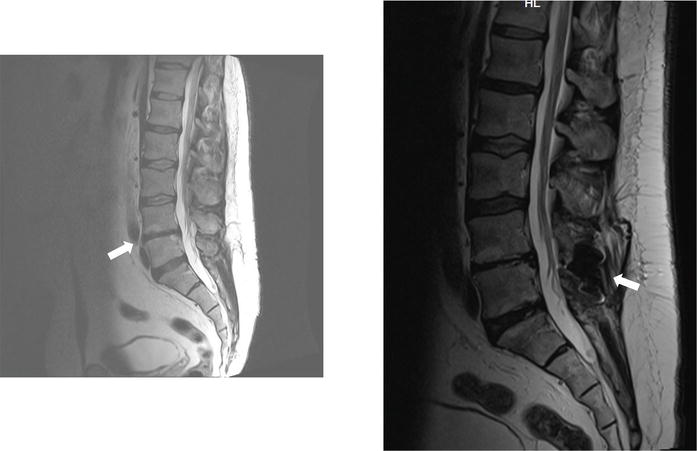
Figure 16.
Lumbar DDD. Preoperative (
10. Final reflections
Of course, most of the spinal disorders described in Section 5 may be treated by means of other surgical techniques; concerning this statement, some observations help both the surgeon and the patient. First, a ‘(at least) second opinion’ will help the patient to take the right decision to manage his/her problem; second, ISD implant may be considered as an ‘intermediate step in the continuum of care for patients with NIC associated with lumbar spinal stenosis’ [16].
In some western countries ISDs are widely implanted by physiatrists and interventional pain specialists; recently, a small series of complications related to ISD implants, in particular, the migration of the spacer in the spinal canal, performed by pain specialists, was reported [17]. Over the last two decades, the industry has promoted the ISD surgical implant and, based upon its presumed ‘easiness of technique’, it forced its use by ‘non-spine surgeons’; the matters of incorrect surgical indication, poor knowledge of the biomechanics of the spinal column, inability to manage potential complications, have rocketed. It has been strongly recommended that ‘spinal instrumentation, however minimally invasive, should be performed by fellowship-trained spine surgeons’ and, in the same way, a consultation with an experienced spine surgeon before an ISD implantation should be performed [17].
As for most lumbar spine surgical procedures, the problem of costs exists for ISD implant too; this directly leads to our (as surgeons) formidable task to conciliate budget-based medicine and the goal of ‘best treatment for the ideal patient’; therefore, settings of clinical assessment, surgical experience, profound knowledge of available spacers, must be managed with skill and simultaneously by the experienced surgeon. This goal will revitalize the somewhat abandoned ‘ancient doctor-patient relationship’ and decrease the high rate of litigation in spinal surgery [18].
Very recently, the experience of ISD implantation was reported as being very satisfying in terms of minimal surgical invasiveness and good clinical outcome [19]; based upon our 20-year ISD-dedicated surgery, we truly share these observations: early in the postoperative course, most of our ISD-implanted patients refer to stand and walk with a straight back after a long time of pain and claudication, and this excellent result usually maintains over time.
Acknowledgments
Our huge thanks run to Dr Susanna USAI (Acting Director, Neurologia 3, Istituto Neurologico ‘Carlo Besta’, Milan, Italy): her acute and stimulating observations are always precious to us.
Conflict of interest
The Author declares no conflict of interest.
References
- 1.
Sénégas J. Lumbar dynamic stabilization with the Wallis implant. Argospine News & Journal. 2009; 21 (2):48-55 - 2.
Kabir SMR, Gupta SR, Casey ATH. Lumbar interspinous spacers; a systematic review of clinical and biomechanical evidence. Spine. 2010; 35 :E1499-E1506 - 3.
Irace C, Giannachi L, Amato V, Corona C. The BacJac interspinous device in the treatment of lumbar spine degenerative disorders: A prospective study and 2-year follow-up results. Journal of Spine. 2014; 3 :163-168 - 4.
Schulte TL, Hurschler C, Haversath M, Liljenqvist U, Bullmann V, Filler TJ, et al. The effect of dynamic, semi-rigid implants on the range of motion of lumbar motion segments after decompression. European Spine Journal. 2008; 17 :1057-1065 - 5.
Kim KA, McDonald M, Pik JHT, Khoueir P, Wang MY. Dynamic intraspinous spacer technology for posterior stabilization: case-control study on the safety, sagittal angulation, and pain outcome al 1-year follow-up evaluation. Neurosurgery Focus. 2007; 22 (1):E7 - 6.
Caporlingua F. (Editorial on): Superion® InterSpinous Spacer treatment of moderate spinal stenosis: 4-year results. Journal of Spine Surgery. 2018; 4 (3):666-667. DOI: 10.21037/jss.2018.08.01 - 7.
Gala RJ, Russo GS, Whang PG. Interspinous implants to treat spinal stenosis. Current Review Musculoskeletal Medicine. 2017; 10 :182-188 - 8.
Giltaij L, Timothy J, Derks M. BacJac interspinous decompression system: another me-too or an improvement? Spinal Surgery News. 2008; 2008 :29-34 - 9.
Pintauro M, Duffy A, Vahedi P, Rymarczuk G, Heller J. Interspinous implants: are the new implants better than the last generation? A review. Current Review in Musculoskeletal Medicine. 2017; 10 :189-198 - 10.
Assietti R, De Falco R. The first multicenter, prospective 6 month follow-up study of 21 patients treated with the Aperius Perclid system. In: 13th European Congress of Neurosurgery – EANS. Glasgow, United Kingdom; 2007. pp. 607-613 - 11.
Karahalios DG, Kaibara T, Porter RW, Kakarla UK, Reyes PM, Baaj AA, et al. Biomechanics of a lumbar interspinous anchor with anterior lumbar interbody fusion. Journal of Neurosurgery Spine. 2010; 12 (4):372-380 - 12.
Plasencia Arriba MA, Maestre C, Martin-Gorrono F, Plasencia P. Analysis of long-term results of lumbar discectomy with and without an interspinous device. International Journal of Spine Surgery. 2022; 16 (4):681-689 - 13.
Barbagallo GM, Olindo G, Corbino L, Albanese V. Analysis of complications in patients treated with the X-Stop Interspinous Process Decompression System: proposal for a novel anatomic scoring system for patient selection and review of the literature. Neurosurgery. 2009; 65 :111-120 - 14.
Verbiest H. Sur certaines forms rares de compression de la queue de cheval. Hommage à Clovis Vincent. Paris: Maloine; 1949. pp. 161-174 - 15.
Schenck CD, Terpstra SES, Moojen WA, van Zwet E, Peul W, Arts MP, et al. Interspinous process device versus conventional decompression for lumbar spinal stenosis: 5-year results of a randomized controlled trial. Journal of Neurosurgery Spine. 2022; 36 :909-917 - 16.
Carl L. Appropriate selection of patients with lumbar spine stenosis for interspinous process decompression with the X STOP device. Neurosurgery Focus. 2007; 22 (1):E5 - 17.
Florence TJ, Say I, Patel KS, Unterberger A, Laiwalla A, Vivas AC, et al. Neurosurgical management of interspinous device complications: a case series. Frontiers in Surgery. 2022; 9 :1-9 - 18.
Irace C. Wrong level (reply to letter). Journal of Neurosurgery Spine. 2011; 12 :689-690 - 19.
Gilbert JW, Christensen B, Matheny S. Interspinous process device clinical practice experience. Journal of Neurosurgery Spine. 2022; 25 :1-2. DOI: 10.3171/2022.7.SPINE22831