Abstract
Pelvic trauma (PT) occurs in 3% of skeletal injuries, presents significant challenges in trauma care. Among severe trauma patients admitted to primary care trauma centers, 10% exhibit pelvic fractures, often resulting from high-energy mechanisms. Pelvic fractures frequently result from high-energy mechanisms, are often associated with multisystem injuries, and can lead to catastrophic bleeding. There is a risk of serious morbidity and mortality in these injuries. According to trauma registries of many countries, unstable pelvic fractures are associated with mortality rates ranging from 8 to 32%. Their severity depends on associated nonpelvic injuries and/or hemorrhagic pelvic injuries. Prehospital and hospital management of severe pelvic trauma requires clear organizational and therapeutic strategies to control bleeding as quickly as possible. Mortality rates remain high, especially in patients with hemodynamic instability, due to rapid bleeding, difficulty in achieving hemostasis and related injuries. For these reasons, a multidisciplinary approach is important in the management of resuscitation, control of bleeding, and treatment of bone injuries, especially in the first hours of trauma. Multimodal treatment approach has become the gold standard in pelvic trauma. These include prehospital use of pelvic binders, appropriate imaging strategy, and appropriate use of surgical or interventional radiological control of bleeding.
Keywords
- pelvic trauma
- pelvic fractures
- bleeding
- shock
- surgery
- trauma
- emergency management
1. Introduction
The pelvis, situated at the center between the lumbar region of the abdomen and the thighs, plays a vital role in supporting the weight of the upper body. Its structure encompasses the osseous pelvis, pelvic cavity, floor, and perineum. Besides its weight-bearing function, the pelvis also redistributes the weight to the lower extremities and provides anchorage for the muscles of the lower limbs and torso. It additionally safeguards the organs within the pelvic and abdominopelvic regions. Pelvic assessments, especially relevant in obstetrics and gynecology, are conducted through various techniques such as the diagonal and obstetric conjugates. Despite being rare, dislocations, hernias, and prolapses related to the pelvis are observed across diverse patient groups [1]. The pelvis serves multiple roles, primarily offering structural support and enabling a range of movements, including standing, walking, and running. Each segment of the pelvis contributes distinct functions, underscoring the importance of understanding each part to fully grasp the pelvis’s overall roles [2, 3]. The pelvis’s bony structure is akin to a ring, comprising the sacrum and the paired innominate bones – the ischium, ilium, and pubis [4]. It encloses the viscera of the gastrointestinal and genitourinary systems. The primary blood supply to the pelvis comes from the internal iliac arteries and their branches. The venous network mirrors the arterial system, forming a plexus along the posterior wall of the pelvis. Bleeding in pelvic fractures usually originates from the venous plexus or the spongy bone, although arterial hemorrhage, which is linked to life-threatening conditions, occurs in a substantial number of instances [5].
2. Mechanisms of pelvic injuries
The predominant causes of pelvic ring fractures are high-energy impacts, such as falls from significant heights, sports accidents, and various forms of road traffic incidents, including those involving pedestrians, motorcyclists, drivers, and bicyclists, as well as incidents where individuals are struck by vehicles [6, 7]. Upon arrival at emergency departments, approximately 10 to 15% of individuals with pelvic fractures are in a state of shock, and about one-third of these patients succumb to their injuries, leading to a recent reported mortality rate of 32% [8]. The primary reasons for these fatalities largely involve uncontrolled hemorrhage and the physiological depletion of the patient.
3. Injury assessment techniques
Upon admission, prompt radiological evaluations are conducted, typically involving supine X-rays for both the pelvis and chest, along with a Focused Assessment with Sonography for Trauma (FAST) abdominal ultrasound examination [9]. However, in cases where the patient’s history, such as a falling on the feet, or physical examination provides strong indications of isolated pelvic trauma, such as pelvic ring deformity, a substantial hematoma altering the perineum’s shape, or bleeding from the rectum or urethra, it is crucial to recognize that FAST has restricted diagnostic efficacy [10]. There’s also a heightened risk of false positives for hemoperitoneum, particularly in the presence of a sizable retroperitoneal hematoma. In such scenarios, a total body spiral Computed Tomography (CT) scan offers superior diagnostic accuracy and can be performed swiftly, typically in under 2 minutes. This rapid and comprehensive imaging is essential in the urgent evaluation of pelvic and perineal trauma (PPT), concurrent with ongoing fluid resuscitation efforts. Ideally, patients should be swiftly transitioned from the CT scanning process to the angioembolization suite, typically within a timeframe of 10 to 20 minutes. Preparations for embolization can be simultaneously arranged in the angiography suite while the CT is being conducted.
4. Management principles for severe pelvic fractures
Treating severe pelvic fractures is a notably complex and critical aspect fort he care of trauma. These fractures often caused by high energy impacts and are typically accompanied by multisystem injuries, leading to potentially life-threatening hemorrhage. The morbidity and mortality associated with these injuries are significant, with reported mortality rates for unstable pelvic fractures ranging from 8 to 32% across various international trauma registries [11, 12, 13, 14, 15, 16]. In-depth discussions on the resuscitation of severely injured patients are available elsewhere. Given the potential for substantial damage to the pelvic vasculature, relying on femoral venous access is often impractical due to concerns that infused fluids may not effectively reach the right atrium. Therefore, it is crucial to place two or more large-bore IntraVenous (IV) catheters (14–18 gauge) in the antecubital fossae or a large-size percutaneous introducer sheath in the subclavian vein to ensure adequate resuscitation for patients with severe pelvic injuries. In instances where peripheral IV catheterization proves unsuccessful, prompt placement of an intraosseous (IO) catheter in the proximal humerus is recommended as a temporary solution to guarantee sufficient IV access. The fluid resuscitation strategy should adhere to the principles of damage control resuscitation. For patients who remain hemodynamically unstable despite initial resuscitation, prioritizing bleeding control is crucial. Rapid identification of the bleeding source is vital, especially in situations where conducting a CT scan is unfeasible. Under such circumstances, pelvic and chest X-rays (CXR), along with Extended Focused Assessment with Sonography for Trauma (EFAST) are the only feasible imaging methods compatible with ongoing resuscitation and urgent decision-making for bleeding control, be it surgical or radiological. If CXR and EFAST exclude extra-pelvic causes of hemorrhagic shock, pelvic angiography is highly likely to reveal active arterial bleeding, necessitating a subsequent body CT scan with intravenous contrast, followed by angiography and embolization. In rare instances of uncontrollable hemorrhagic shock, angiography and embolization might be required directly following CXR and E-FAST to address potential massive non-pelvic hemorrhage. When pelvic trauma is accompanied by hemoperitoneum, determining the bleeding source becomes more complex, often depending on the stability of the pelvic fracture. Typically, the source of active bleeding is abdominal (70%) in cases of stable pelvic fractures and pelvic (56%) in cases of unstable fractures [17], though uncertainties persist in both scenarios. The extent of hemoperitoneum also plays a crucial role, as significant hemoperitoneum usually indicates major intra-abdominal bleeding that necessitates surgical intervention. Opting for angiographic embolization to control pelvic bleeding also facilitates the management of concurrent intra-abdominal bleeding sources, such as those resulting from hepatic, splenic, or renal injuries. The relevance of pelvic CXRs, in this context, hinges on the patient’s hemodynamic stability and the presence of extra-pelvic (primarily thoracic and/or abdominal) bleeding sources. For hemodynamically stable patients, pelvic CXRs are less influential in patient management since normal findings rule out major pelvic injuries as the source of bleeding but do not discount the presence of pelvic fractures, which may be identified through CT scans.
In managing abdominal digestive tract injuries, standard treatment protocols are followed. For patients who have PPT, conducting a digital rectal examination is crucial; the presence of blood indicates a potential rectal injury, even if not visibly apparent. Diligent investigation for subperitoneal rectal injuries is vital, as undetected injuries can lead to a mortality rate of up to 50% when sepsis develops in patients with open pelvic fractures [18]. While monitoring for improvement in the patient’s overall condition, they should be kept in intensive care, utilizing transcondylar leg traction and Ganz® clamp pelvic immobilization. The use of muscle relaxants (curarization) is essential for the effectiveness of external orthopedic procedures, ensuring the maintained reduction of the fracture and preventing the upward movement of a dislocated hemipelvis. Subsequent treatment of pelvic bony injuries involves iliosacral screw fixation for posterior fractures, occasionally in conjunction with realignment of the symphysis pubis. The ease of delayed percutaneous fracture fixation is enhanced when the pelvic ring fractures are preliminarily reduced [19].
5. Treatment approaches for pelvic injuries
The treatment for pelvic injuries encompasses a range of methods including pelvic binding, angiography with embolization, surgical stabilization, care for concurrent injuries, and the exploration of newer therapeutic approaches such as the use of resuscitative endovascular balloon occlusion of the aorta (REBOA) and the integration of operative and angiography facilities.
6. Pelvic binding
For the temporary stabilization of unstable pelvic fractures, the application of noninvasive external compression, known as pelvic binding (Figure 1), is advised. This method offers multiple advantages: it prevents further movement of the pelvis, decreases the pelvic volume which in turn helps in reducing bleeding, and alleviates discomfort for the patient [20]. Quick stabilization is possible through the circumferential wrapping of a bedsheet around the patient’s pelvis, specifically positioned at the level of the greater trochanter. It’s crucial to ensure the wrap is placed accurately for maximum effectiveness. While there are various commercially available devices designed for pelvic binding, there is not conclusive evidence to suggest that these are superior to the use of a simple bedsheet. Some commercial devices might offer benefits in terms of ease of application and consistency [21], but they may also restrict access to the groin area which is necessary for procedures like angiography or REBOA placement. In contrast, a bedsheet can be modified to provide necessary access while still maintaining the effectiveness of the wrap. Using Kelly clamps to secure the bedsheet can help reduce the risk of skin necrosis, a common issue with knots, but it’s important to note that these clamps might create artifacts in CT scans. This issue can be circumvented by opting for commercially available zip ties as an alternative for securing the wrap.

Figure 1.
Pelvic binding.
7. Extraperitoneal pelvic packing (EPP)
First introduced in literature in 1994 [22], EPP has gained increasing clinical application since the year 2000 [23, 24, 25, 26, 27, 28]. EPP is recognized for its effectiveness in stabilizing patients who continue to be unstable despite traditional management methods, including skeletal fixation and arteriography. However, there is a lack of consensus regarding its role, as evidenced by differing American and European guidelines. In the United States, EPP is regarded as an effective method for hemorrhage control, but primarily as a secondary strategy following embolization, with a Grade III evidence level [21]. Conversely, European guidelines suggest an earlier use of EPP in patients who continue to bleed despite successful pelvic ring fixation or following surgical bleeding or embolization control [29]. EPP, however, is an invasive procedure, and there have been reports of surgical site infections associated with its use [26, 30], particularly when performed in trauma bay settings. Additionally, there is an increased risk of developing abdominal compartment syndrome(ACS) [24, 31] and the potential need for subsequent re-operation and removal of the packing within 24 to 48 hours.
8. Angiography and embolization
The majority of bleeding associated with pelvic fractures originates from veins; however, arterial hemorrhage, when it occurs, often gives rise to being hemodynamic instable and an increased risk of blood loss. Transcatheter Arterial Embolization (TAE) is recognized as the most effective treatment for managing pelvic fractures accompanied by arterial bleeding. Newest systematic reviews of TAE in pelvic fractures show an effectivity rate ranging from 81 to 100% in controlling arterial hemorrhage, resulting in a significant reduction in the need for blood transfusions and a decrease in mortality rates associated with pelvic bleeding [32]. Indications for TAE are ongoing hemodynamic instability, post-resuscitation and pelvic binding, the presence of a contrast enhancement on CT scans, a visible large pelvic hematoma on CT, and advanced patient age [21]. Timely execution of TAE is crucial, as delays have been associated with increased mortality risks [33, 34], presenting a critical challenge even in well-equipped trauma centers [35]. There is considerable interest in establishing the optimal sequence of interventions for controlling hemorrhage in hemodynamically unstable patients with pelvic fractures.
9. Resuscitative endovascular balloon occlusion of the aorta (REBOA)
REBOA is recognized as an innovative and effective method for controlling bleeding in patients experiencing hemorrhagic shock. Specifically, the deployment of the balloon in Zone 3 has been suggested as a viable option for managing pelvic hemorrhage [36, 37]. Studies have indicated that the use of REBOA in Zone 3, in contrast to Zone 1, significantly enhances survival rates by effectively controlling pelvic arterial blood flow [38]. Despite its potential, REBOA is not widely available, and some research has pointed to its association with serious complications, including ischemia-reperfusion syndrome, acute kidney injury, limb amputation, and an increase in mortality rates [39].
10. Operative stabilization: external pelvic fixation in hemodynamically unstable pelvic injuries
The biomechanics of pelvic ring injuries and the specific nature of the trauma largely dictate the necessity for external fixation [40, 41]. For patients with hemodynamically unstable pelvic ring injury, temporary stabilization is essential to prevent additional hemorrhage and to facilitate hemorrhage control methods such as angiography and pelvic packing [40, 42, 43, 44, 45]. The fundamental objectives of immediate external pelvic fixation encompass diminishing intrapelvic volume in injuries resembling an “open book” configuration to mitigate the space for retroperitoneal bleeding and offering a steadfast counterpressure against lap sponges employed in pelvic packing. Notably, pelvic packing is ineffective without sufficient counterpressure from the posterior pelvic structures, necessitating external fixation in cases of unstable pelvic ring disruptions [41, 46, 47]. Determining the appropriate type of external fixation, often termed “damage control” fixation, for unstable pelvic ring injuries is a complex decision-making process [40]. The indication of pelvic external fixation are guided by the Young & Burgess fracture classification system and defined the technique [40, 48]. Anterior posterior compression and lateral compression injuries are typically addressed with anterior stabilization frames, employing either iliac crest or supra-acetabular Schanz pin application. The iliac crest approach is less technically demanding and allows for quicker application, but Schanz pins in the iliac crest have a lower resistance to pull-out, increasing the risk of fixation failure. In contrast, supra-acetabular frames, necessitating meticulous pin placement under radiographic control, offer higher pull-out resistance due to the robust supra-acetabular surgical corridor [40]. For vertically unstable pelvic ring disruptions, such as “vertical shear” (VS) injuries, a posterior C-clamp is preferred [23, 49, 50, 51, 52, 53]. Trauma surgeons must be cognizant of the inherent risks and technical complexities associated with the C-clamp, including a steep learning curve and the necessity for experienced application [54, 55]. Contraindications for using a pelvic C-clamp include complex sacral fractures, iliac wing fractures, and lateral compression-type injuries [40].
11. Definitive internal pelvic fixation
The optimal timing for conclusively addressing unstable pelvic ring injuries remains a topic of ongoing discussion in the medical community [56, 57, 58, 59, 60, 61, 62, 63]. Generally, experts agree that individuals undergoing severe traumatic-hemorrhagic shock due to disruptions in the pelvic ring are typically not deemed appropriate candidates for an early definitive intervention. This is mainly because of the heightened risk of mortality linked to excessive bleeding and the potentially fatal combination of coagulopathy, acidosis, and hypothermia [64, 65]. An impactful multicenter cohort study emphasized that early fixation of pelvic fractures, especially within the initial or second day post-injury, results in significantly greater blood loss and heightened levels of interleukin (IL-6 and IL-8) in the serum, indicating an intensified systemic inflammatory response in polytrauma patients [66]. It was also noted that the early and brief period of initial pelvic stabilization contributed to a lower incidence of multiple organ failure (MOF) and reduced mortality rates [67]. However, complication rates post-injury were observed to rise when the definitive fixation of the pelvic ring was performed between the second and fourth days post-injury, compared to delaying the surgery until the sixth to eighth day [68]. The prevailing perspective endorses the strategy of initial ‘damage control’ external fixation for hemodynamically unstable pelvic ring injuries, followed by delayed definitive internal fixation after the fourth day, post successful resuscitation [40, 42, 69, 70, 71, 72, 73, 74]. This approach, along with the application of classification systems, provides guidance in categorizing patients with unstable polytrauma and pelvic ring injuries who necessitate damage control measures, in contrast to those who are stable or borderline stable and may be suitable for an early definitive pelvic fracture intervention [59, 65]. In this context, various observational studies from the orthopedic trauma group at MetroHealth in Cleveland have shown that early fixation of pelvic fractures within 24 hours of admission in stable or borderline resuscitated patients can significantly lower the risk of complications and enhance overall outcomes [57, 59, 62, 63]. Recently, an international consensus group proposed a new definition of polytrauma, based on the severity of the injury and physiological parameter disturbances [75]. This new definition, along with recently established grading systems [59], may further refine the criteria for determining the optimal timing for definitive pelvic fracture fixation, pending additional validation studies (Figure 2).
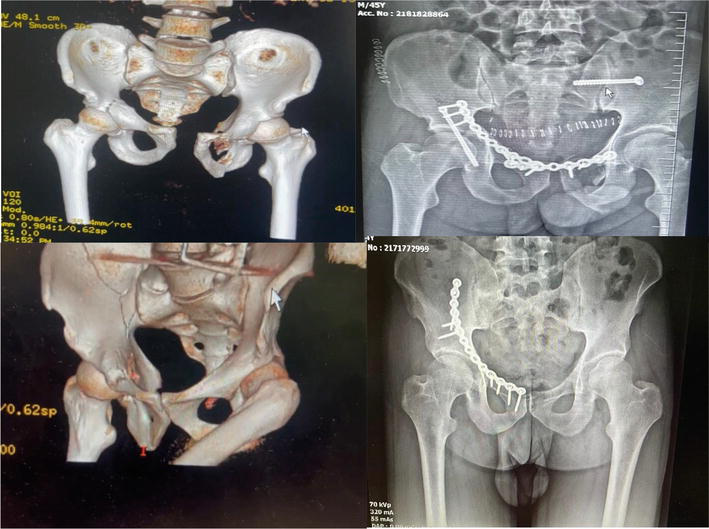
Figure 2.
Pelvic fracture with separation of pubic ramus and open reduction and fixed with plate and screws.
12. Morbidity, mortality, and outcomes in pelvic trauma
Patients with open pelvic trauma (PT) frequently encounter complications that markedly impact functionality, giving rise to chronic consequences such as urinary and fecal incontinence, impotence, dyspareunia, residual physical disabilities, perineal and pelvic abscesses, chronic pain, and vascular complications such as embolism or thrombosis [6, 76]. It’s noteworthy that the highest proportion of deaths (44.7%) occurs on the day of the trauma itself. Factors closely associated with increased mortality rates include older age, the severity of the injury as measured by the Injury Severity Score (ISS), instability of the pelvic ring, the extent and contamination of open wounds, rectal injuries, fecal diversion, the number of blood units transfused, head injury severity as per the Abbreviated Injury Scale (AIS), and the base deficit upon admission [7, 76].
A recent study has highlighted the positive impact of a multidisciplinary approach on both performance and patient outcomes [7]. Initially, a well-defined decision-making algorithm significantly reduced the time between hospital arrival and bleeding control in the theater using Pelvic Packing Procedures (PPP) [7]. Additionally, the implementation of a massive hemorrhage protocol substantially decreased the pre-transfusion administration of fluids and rationalized the use of packed red cells and fresh frozen plasma at a ratio of 2:1, commencing within the initial hours post-injury [7]. The involvement of specialized pelvic orthopedic surgeons demonstrated a significant improvement (p = 0.004) in the proportion of patients undergoing definitive repairs for unstable pelvic fractures, leading to enhanced patient outcomes [7]. Similar observations underscoring the importance of adhering to established guidelines were reported by Balogh et al. [77] and were subsequently reinforced by the multi-institutional trial led by Costantini et al. [8].
13. Conclusion
This chapter has highlighted key advancements in managing pelvic trauma, focusing on combatting profuse bleeding and shock, and detailing both emergency and definitive treatment strategies. Our findings emphasize the importance of immediate interventions, such as the use of pelvic binders and tranexamic acid, which have proven critical in reducing the mortality rates associated with these injuries. The study further demonstrates the effectiveness of an integrated approach combining surgical and interventional radiology techniques for rapid hemorrhage control, significantly enhancing patient stabilization.
Moreover, we have outlined improvements in definitive treatment approaches, advocating for a patient-specific strategy that optimizes mechanical stability and physiological recovery. The incorporation of a multidisciplinary framework underscores the necessity of cross-specialty collaboration for effective pelvic trauma management.
In summary, this research contributes significantly to the existing body of knowledge on pelvic trauma care, offering innovative strategies for emergency intervention and definitive treatment that promise to improve patient outcomes in trauma care settings.
References
- 1.
DeSilva JM, Rosenberg KR. Anatomy, development, and function of the human pelvis. The Anatomical Record (Hoboken). 2017; 300 (4):628-632 - 2.
Aldabe D, Hammer N, Flack NAMS, Woodley SJ. A systematic review of the morphology and function of the sacrotuberous ligament. Clinical Anatomy. 2019; 32 (3):396-407 - 3.
Matsutani H, Nakai G, Yamada T, Yamamoto K, Ohmichi M, Narumi Y. Diversity of imaging features of ovarian sclerosing stromal tumors on MRI and PET-CT: A case report and literature review. Journal of Ovarian Research. 2018; 11 (1):101 - 4.
Marx J, Walls R, Hockberger R, Biros M, et al, editors. Rosen’s Emergency Medicine - Concepts and Clinical Practice. Vol. 2014. Philadelphia, PA: Elsevier/Saunders; 2014. pp. 656-671 - 5.
Cook RE, Keating JF, Gillespie I. The role of angiography in the management of haemorrhage from major fractures of the pelvis. Journal of Bone and Joint Surgery. British Volume (London). 2002; 84 (2):178-182 - 6.
Arvieux C, Thony F, Broux C, et al. Current management of severe pelvic and perineal trauma. Journal of Visceral Surgery. 2012; 149 :e227-e238 - 7.
Perkins ZB, Maytham GD, Koers L, Bates P, Brohi K, Tai NR. Impact on outcome of a targeted performance improvement programme in haemodynamically unstable patients with a pelvic fracture. The Bone & Joint Journal. 2014; 96-B :1090-1097 - 8.
Costantini TW, Coimbra R, Holcomb JB, et al. Current management of hemorrhage from severe pelvic fractures: Results of an American Association for the Surgery of Trauma multi-institutional trial. Journal of Trauma and Acute Care Surgery. 2016; 80 :717-723. discussion 23-25 - 9.
Arvieux C, Cardin N, Létoublon C. La laparotomie écourtée pour le traitement des traumatismes abdominaux sévères. In: Annales de Chirurgie. Vol. 131, No. 5. Elsevier Masson; May 2006. pp. 342-346 - 10.
Ballard RB, Rozycki GS, Newman PG, et al. An algorithm to reduce the incidence of false-negative FAST examinations in patients at high risk for occult injury. Focused assessment for the sonographic examination of the trauma patient. Journal of the American College of Surgeons. 1999; 189 :145-150 [discussion 141-150] - 11.
Giannoudis PV, Grotz MRW, Tzioupis C, et al. Prevalence of pelvic fractures, associated injuries, and mortality: The United Kingdom perspective. The Journal of Trauma. 2007; 63 (4):875-883 - 12.
Hauschild O, Strohm PC, Culemann U, et al. Mortality in patients with pelvic fractures: Results from the German pelvic injury register. The Journal of Trauma. 2008; 64 (2):449-455 - 13.
Yoshihara H, Yoneoka D. Demographic epidemiology of unstable pelvic fracture in the United States from 2000 to 2009: Trends and in-hospital mortality. Journal of Trauma and Acute Care Surgery. 2014; 76 (2):380-385 - 14.
Vaidya R, Scott AN, Tonnos F, et al. Patients with pelvic fractures from blunt trauma. What is the cause of mortality and when? American Journal of Surgery. 2016; 211 (3):495-500 - 15.
Costantini TW, Coimbra R, Holcomb JB, et al. Current management of hemorrhage from severe pelvic fractures. Journal of Trauma and Acute Care Surgery. 2016; 80 (5):717-725 - 16.
Inaba K, Sharkey PW, Stephen DJG, et al. The increasing incidence of severe pelvic injury in motor vehicle collisions. Injury. 2004; 35 (8):759-765 - 17.
Eastridge BJ, Starr A, Minei JP, O’Keefe GE, Scalea TM. The importance of fracture pattern in guiding therapeutic decision-making in patients with hemorrhagic shock and pelvic ring disruptions. The Journal of Trauma. 2002; 53 :446-450 - 18.
Dente CJ, Feliciano DV, Rozycki GS, et al. The outcome of open pelvic fractures in the modern era. American Journal of Surgery. 2005; 190 :830-835 - 19.
Nordin J, Tonetti J. Les fractures et disjonctions de l’anneau pelvien de l’adulte. Paris: Monographie de la Sofcot; 2006. pp. 31-34 - 20.
Bakhshayesh P, Boutefnouchet T, Tötterman A. Effectiveness of non invasive external pelvic compression: A systematic review of the literature. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. 2016; 24 :73 - 21.
Cullinane DC, Schiller HJ, Zielinski MD, et al. Eastern Association for the Surgery of trauma practice management guidelines for hemorrhage in pelvic fracture– Update and systematic review. The Journal of Trauma. 2011; 71 (6):1850-1868 - 22.
Pohlemann T, Bosch U, Gänsslen A, Tscherne H. The Hanover experience in management of pelvic fractures. Clinical Orthopaedics. 1994; 305 :69-80 - 23.
Ertel W, Eid K, Keel MTO. Therapeutical strategies and outcome of polytraumatized patients with pelvic injuries. European Journal of Trauma. 2000; 26 :278-286 - 24.
Ertel W, Keel M, Eid K, Platz A, Trentz O. Control of severe hemorrhage using C-clamp and pelvic packing in multiply injured patients with pelvic ring disruption. Journal of Orthopaedic Trauma. 2001; 15 (7):468-474 - 25.
Smith WR, Moore EE, Osborn P, et al. Retroperitoneal packing as a resuscitation technique for hemodynamically unstable patients with pelvic fractures: Report of two representative cases and a description of technique. The Journal of Trauma. 2005; 59 (6):1510-1514 - 26.
Cothren CC, Osborn PM, Moore EE, Morgan SJ, Johnson JL, Smith WR. Preperitonal pelvic packing for hemodynamically unstable pelvic fractures: A paradigm shift. The Journal of Trauma. 2007; 62 (4):834-839 [discussion 839-842] - 27.
Pohlemann T, Gansslen A, Hufner T, Tscherne H. EXtraperitoneal packing at laparotomy. In: Abstract OTA-AAST Annual Meeting. 2000 - 28.
Giannoudis PV, Pape HC. Damage control orthopaedics in unstable pelvic ring injuries. Injury. 2004; 35 (7):671-677 - 29.
Rossaint R, Bouillon B, Cerny V, et al. Management of bleeding following major trauma: An updated European guideline. Critical Care. 2010; 14 (2):R52 - 30.
Tötterman A, Madsen JE, Skaga NO, Røise O. Extraperitoneal pelvic packing: A salvage procedure to control massive traumatic pelvic hemorrhage. The Journal of Trauma. 2007; 62 (4):843-852 - 31.
Ertel W, Oberholzer A, Platz A, Stocker R, Trentz O. Incidence and clinical pattern of the abdominal compartment syndrome after “damage control” laparotomy in 311 patients with severe abdominal and/or pelvic trauma. Critical Care Medicine. 2000; 28 (6):1747-1753 - 32.
Papakostidis C, Kanakaris N, Dimitriou R, et al. The role of arterial embolization in controlling pelvic fracture haemorrhage: A systematic review of the literature. European Journal of Radiology. 2012; 81 (5):897-904 - 33.
Schwartz DA, Medina M, Cotton BA, et al. Are we delivering two standards of care for pelvic trauma? Availability of angioembolization after hours and on weekends increases time to therapeutic intervention. Journal of Trauma and Acute Care Surgery. 2014; 76 (1):134-139 - 34.
Tanizaki S, Maeda S, Matano H, et al. Time to pelvic embolization for hemodynamically unstable pelvic fractures may affect the survival for delays up to 60 min. Injury. 2014; 45 (4):738-741 - 35.
Tesoriero R, Bruns B, Narayan M, et al. Angiographic embolization for hemorrhage following pelvic fracture: Is it “time” for a paradigm shift? Journal of Trauma and Acute Care Surgery. 2017; 82 (1):18-26 - 36.
Brenner M, Teeter W, Hoehn M, Pasley J, Hu P, Yang S, et al. Use of resuscitative endovascular balloon occlusion of the aorta for proximal aortic control in patients with severe hemorrhage and arrest. JAMA Surgery. 2018; 153 :130-135 - 37.
Morrison JJ, Percival TJ, Markov NP, Villamaria C, Scott DJ, Saches KA, et al. Aortic balloon occlusion is effective in controlling pelvic hemorrhage. The Journal of Surgical Research. 2012; 177 :341-347 - 38.
Do WS, Forte DM, Sheldon RR, Weiss JB, Barron MR, Sokol KK, et al. Preperitoneal balloon tamponade and resuscitative endovascular balloon occlusion of the aorta: Alternatives to open packing for pelvic-associated hemorrhage. Journal of Trauma and Acute Care Surgery. 2019; 87 :18-26 - 39.
DuBose JJ, Scalea TM, Brenner M, Skiada D, Inaba K, Cannon J, et al. The AAST prospective aortic occlusion for resuscitation in trauma and acute care surgery (AORTA) registry: Data on contemporary utilization and outcomes of aortic occlusion and resuscitative balloon occlusion of the aorta (REBOA). Journal of Trauma and Acute Care Surgery. 2016; 81 :409-419 - 40.
Stahel PF, Mauffrey C, Smith WR, et al. External fixation for acute pelvic ring injuries: Decision making and technical options. Journal of Trauma and Acute Care Surgery. 2013; 75 :882-887 - 41.
Rommens PM, Hofmann A, Hessmann MH. Management of Acute Hemorrhage in pelvic trauma: An overview. European Journal of Trauma and Emergency Surgery. 2010; 36 :91-99 - 42.
Marzi I, Lustenberger T. Management of Bleeding Pelvic Fractures. Scandinavian Journal of Surgery. 2014; 103 :104-111 - 43.
Abrassart S, Stern R, Peter R. Unstable pelvic ring injury with hemodynamic instability: What seems the best procedure choice and sequence in the initial management? Orthopaedics & Traumatology, Surgery & Research. 2013; 99 :175-182 - 44.
Esmer E, Esmer E, Derst P, Schulz M, Siekmann H, Delank KS, et al. Influence of external pelvic stabilization on hemodynamically unstable pelvic fractures. Der Unfallchirurg. 2017; 120 :312-319 - 45.
Poenaru DV, Popescu M, Anglitoiu B, Popa I, Andrei D, Birsasteanu F. Emergency pelvic stabilization in patients with pelvic posttraumatic instability. International Orthopaedics. 2015; 39 :961-965 - 46.
Burlew CC, Moore EE, Smith WR, et al. Preperitoneal pelvic packing/external fixation with secondary angioembolization: Optimal care for life-threatening hemorrhage from unstable pelvic fractures. Journal of the American College of Surgeons. 2011; 212 :628-635. discussion 35-37 - 47.
Osborn PM, Smith WR, Moore EE, et al. Direct retroperitoneal pelvic packing versus pelvic angiography: A comparison of two management protocols for haemodynamically unstable pelvic fractures. Injury. 2009; 40 :54-60 - 48.
Burgess A. Invited commentary: Young-Burgess classification of pelvic ring fractures: Does it predict mortality, transfusion requirements, and non-orthopaedic injuries? Journal of Orthopaedic Trauma. 2010; 24 :609 - 49.
Lustenberger T, Fau MC, Benninger E, Fau BE, Lenzlinger PM, Lenzlinger Pm F, et al. C-clamp and pelvic packing for control of hemorrhage in patients with pelvic ring disruption. Journal of Emergencies, Trauma, and Shock. 2011; 4 :477-482 - 50.
Heini PF, Witt J, Ganz R. The pelvic C-clamp for the emergency treatment of unstable pelvic ring injuries. A report on clinical experience of 30 cases. Injury. 1996; 27 (Suppl. 1):S-A38-S-A45 - 51.
Pohlemann T, Culemann U, Tosounidis G, Kristen A. Application of the pelvic C-clamp. Der Unfallchirurg. 2004; 107 :1185-1191 - 52.
Tiemann AH, Schmidt C, Gonschorek O, Josten C. Use of the “c-clamp” in the emergency treatment of unstable pelvic fractures. Zentralblatt für Chirurgie. 2004; 129 :245-251 - 53.
Witschger P, Heini P, Ganz R. Pelvic clamps for controlling shock in posterior pelvic ring injuries. Application, biomechanical aspects and initial clinical results. Der Orthopäde. 1992; 21 :393-399 - 54.
Koller H, Balogh ZJ. Single training session for first time pelvic C-clamp users: Correct pin placement and frame assembly. Injury. 2012; 43 :436-439 - 55.
Koller H, Keil P, Seibert F. Individual and team training with first time users of the pelvic C-clamp: Do they remember or will we need refresher trainings? Archives of Orthopaedic and Trauma Surgery. 2013; 133 :343-349 - 56.
Balbachevsky D, Belloti JC, Doca DG, et al. Treatment of pelvic fractures—A national survey. Injury. 2014; 45 (Suppl. 5):S46-S51 - 57.
Childs BR, Nahm NJ, Moore TA, Vallier HA. Multiple procedures in the initial surgical setting: When do the benefits outweigh the risks in patients with multiple system trauma? Journal of Orthopaedic Trauma. 2016; 30 :420-425 - 58.
Enninghorst N, Toth L, King KL, McDougall D, Mackenzie S, Balogh ZJ. Acute definitive internal fixation of pelvic ring fractures in polytrauma patients: A feasible option. The Journal of Trauma. 2010; 68 :935-941 - 59.
Nahm NJ, Moore TA, Vallier HA. Use of two grading systems in determining risks associated with timing of fracture fixation. Journal of Trauma and Acute Care Surgery. 2014; 77 :268-279 - 60.
Pape HC, Tornetta P 3rd, Tarkin I, Tzioupis C, Sabeson V, Olson SA. Timing of fracture fixation in multitrauma patients: The role of early total care and damage control surgery. The Journal of the American Academy of Orthopaedic Surgeons. 2009; 17 :541-549 - 61.
Schreiber VM, Tarkin IS, Hildebrand F, et al. The timing of definitive fixation for major fractures in polytrauma–a matched-pair comparison between a US and European level I centres: Analysis of current fracture management practice in polytrauma. Injury. 2011; 42 :650-654 - 62.
Vallier HA, Cureton BA, Ekstein C, Oldenburg FP, Wilber JH. Early definitive stabilization of unstable pelvis and acetabulum fractures reduces morbidity. The Journal of Trauma. 2010; 69 :677-684 - 63.
Vallier HA, Moore TA, Como JJ, et al. Complications are reduced with a protocol to standardize timing of fixation based on response to resuscitation. Journal of Orthopaedic Surgery and Research. 2015; 10 :155 - 64.
Stahel PF, Moore EE, Schreier SL, Flierl MA, Kashuk JL. Transfusion strategies in postinjury coagulopathy. Current Opinion in Anaesthesiology. 2009; 22 :289-298 - 65.
Pape HC, Giannoudis PV, Krettek C, Trentz O. Timing of fixation of major fractures in blunt polytrauma: Role of conventional indicators in clinical decision making. Journal of Orthopaedic Trauma. 2005; 19 :551-562 - 66.
Pape HC, Griensven MV, Hildebrand FF, et al. Systemic inflammatory response after extremity or truncal fracture operations. The Journal of Trauma. 2008; 65 :1379-1384 - 67.
Probst C, Probst T, Gaensslen A, Krettek C, Pape HC. Timing and duration of the initial pelvic stabilization after multiple trauma in patients from the German trauma registry: Is there an influence on outcome? The Journal of Trauma. 2007; 62 :370-377. discussion 6-7 - 68.
Pape H, Stalp M, Griensven M, Weinberg A, Dahlweit M, Tscherne H. Optimal timing for secondary surgery in polytrauma patients: An evaluation of 4314 serious-injury cases. Der Chirurg. 1999; 70 :1287-1293 - 69.
Spanjersberg WR, Knops SP, Schep NW, van Lieshout EM, Patka P, Schipper IB. Effectiveness and complications of pelvic circumferential compression devices in patients with unstable pelvic fractures: A systematic review of literature. Injury. 2009; 40 :1031-1035 - 70.
Halawi MJ. Pelvic ring injuries: Emergency assessment and management. Journal of Clinical Orthopaedics and Trauma. 2015; 6 :252-258 - 71.
Chu CH, Tennakoon L, Maggio PM, Weiser TG, Spain DA, Staudenmayer KL. Trends in the management of pelvic fractures, 2008-2010. The Journal of Surgical Research. 2016; 202 :335-340 - 72.
D’Alleyrand JC, O’Toole RV. The evolution of damage control orthopedics: Current evidence and practical applications of early appropriate care. The Orthopedic Clinics of North America. 2013; 44 :499-507 - 73.
Katsoulis E, Giannoudis PV. Impact of timing of pelvic fixation on functional outcome. Injury. 2006; 37 :1133-1142 - 74.
Pape HC, Giannoudis P, Krettek C. The timing of fracture treatment in polytrauma patients: Relevance of damage control orthopedic surgery. American Journal of Surgery. 2002; 183 :622-629 - 75.
Pape HC, Lefering R, Butcher N, et al. The definition of polytrauma revisited: An international consensus process and proposal of the new ‘Berlin definition’. Journal of Trauma and Acute Care Surgery. 2014; 77 :780-786 - 76.
Grotz MR, Allami MK, Harwood P, Pape HC, Krettek C, Giannoudis PV. Open pelvic fractures: Epidemiology, current concepts of management and outcome. Injury. 2005; 36 :1-13 - 77.
Balogh Z, Caldwell E, Heetveld M, et al. Institutional practice guidelines on management of pelvic fracture-related hemodynamic instability: Do they make a difference? The Journal of Trauma. 2005; 58 :778-782