Abstract
Acute primary patellar dislocation can occur due to high-energy trauma or be associated with facilitating factors. Following a comprehensive physical examination, computerized tomography and magnetic resonance imaging are necessary, along with anteroposterior and lateral knee radiographs, to diagnose additional injuries and assess underlying facilitating factors. Surgical treatments take precedence in the presence of facilitating factors such as patella alta, increased tibial tuberosity-trochlear groove distance, trochlear dysplasia, increased patellar tilt, and the presence of osteochondral fractures. However, in the absence of these factors, conservative treatment is usually sufficient. Additionally, there is no clear consensus on which surgical strategy to use in the approach to the first dislocation, considering the possible variability in the location of medial patellofemoral ligament (MPFL) injury and the ultimate presence of predisposing factors for patellar instability. While MPFL reconstruction may theoretically be more reliable than repair, there is no clear evidence on whether bone abnormalities should be corrected after the first patellar dislocation.
Keywords
- patellar dislocation
- treatment
- medial patellofemoral ligament
- reconstruction
- repair
- patellar instability
1. Introduction
Patellar dislocations account for an estimated 2–3% of all orthopedic cases involving the knee joint. The average annual incidence of the first patellar dislocation is 5.8 cases per 100,000 individuals, with a notably higher prevalence among adolescents and the physically active population [1, 2]. Patellar dislocation is more frequently observed in females, and athletes under 20 constitute a risky population [3, 4]. Dislocation typically occurs through a noncontact rotational trauma or a direct impact on the lateral aspect of the knee during flexion, leading to external rotation of the tibia and internal rotation of the femur, resulting in patellar displacement [3, 5]. Lateral dislocations are the most commonly encountered. Medial patellar dislocations are generally iatrogenic, often caused by inappropriate lateral retinacular release or excessive medialization of the tibial tubercle [6]. Rates of recurrence following the primary patellar dislocation have been documented to range from 15% to 44% [1, 7]. The injury to the medial patellofemoral ligament (MPFL) is universally recognized as the primary factor in recurrent instability. The MPFL, providing approximately 50–60% of the restraining force, is the main restraint against lateral patellar displacement [8, 9].
Patellar dislocation can occur not only as a result of high-energy trauma but also due to low-energy trauma facilitated by underlying contributing factors [4]. These facilitating factors include patella alta, trochlear dysplasia, increased patellar tilt, and an increased tibial tuberosity-trochlear groove (TT-TG) distance [10]. Additionally, coronal plane deformities such as genu varum and genu valgum, as well as torsional (rotational) deformities, can create a predisposition for patellar dislocation [11]. Conditions characterized by hypermobility, such as Ehlers-Danlos syndrome, may also lead to the development of patellofemoral instability [12]. Understanding all these factors is crucial in treatment planning. Studies have shown that in patients with underlying facilitating factors, the risk of dislocation recurrence is twice as high compared to those without such factors [13]. There are also studies indicating a sixfold increased risk of recurrent dislocation in cases where contralateral patellar dislocation is present [4].
2. Anatomy
The MPFL has a broad insertion, encompassing the medial superior half of the patella and the most distal aspect of the vastus medialis obliquus (VMO) insertion. It is positioned 1.9 mm anterior and 3.8 mm distal to the adductor tubercle, and 10.6 mm proximal and 8.8 mm posterior to the medial epicondyle [14]. The role of the MPFL as the primary patellar stabilizer within the initial 30° of knee flexion has been clearly delineated. In this early flexion phase, the MPFL contributes 50–60% of medial restraint against lateral subluxation, while additional patellar stability is provided by the trochlear groove during deeper knee flexion [15]. Variations in trochlear morphology have the potential to predispose the patella to maltracking and, in severe cases, gross subluxation or dislocation, thus exerting an impact on the recurrence of patellar instability [16].
The lateralization of the TT, arising from the lateral aspect of the proximal tibia, can influence patellar tracking. Factors such as increased tibial external rotation, severe genu valgum, or heightened femoral anteversion, resulting in a relative increase in femoral internal rotation, may contribute to a dramatic change in the Q-angle. This alteration creates a lateralized vector with quadriceps activation, directly affecting the patellofemoral articulation [17]. In cases of an incompetent MPFL, immediate effects in early flexion can occur, leading to patellar subluxation and recurrent dislocations, directly impacting the patellofemoral articulation.
3. Clinical evaluation
Acute patellar dislocation episodes may result from direct trauma or noncontact injuries, causing a sensation of instability or a pop. Spontaneous reduction commonly occurs, but if needed, a reduction maneuver involves gently extending the knee while applying medial force [18]. In the acute setting, physical examination can be challenging due to pain, soft-tissue swelling, and joint hemarthrosis. A significant hemarthrosis can occur, accompanied by medial knee pain indicating damage to the MPFL, as well as lateral knee pain arising from a contusion of the patella against the lateral femoral condyle. The sensitivity over the femoral attachment site of the medial patellofemoral ligament is referred to as the “Bassett sign” [19].
The patellar apprehension test involves applying a laterally directed force to the knee while it is in 20° to 30° of flexion. The test is considered positive if the quadriceps involuntarily contract or if the patient experiences a sensation of apprehension [20]. Conducted with the knee fully extended and quadriceps relaxed, the patellar glide test involves dividing the patella into four quadrants along its width. The examiner then passively translates the patella medially and laterally. A lateral patellar glide of grade 3 or 4 indicates medial soft-tissue insufficiency, and attention should be given to any side-to-side difference [21]. The patellar tilt test, performed with the knee in full extension, assesses the ability to raise the lateral facet. Inability to achieve at least a neutral position during this test is indicative of a tight lateral retinaculum or iliotibial band [22]. The most comprehensive assessment of patellar tracking can be achieved through active knee range of motion evaluation in a seated position. The presence of the J-sign is considered an excessive lateral translation of the patella due to its separation from the trochlear groove in extension, and it is often associated with patella alta and trochlear dysplasia [23]. The presence of crepitus may indicate accompanying osteochondral damage.
4. Radiological evaluation
A standard radiographic series, including standing anteroposterior, lateral with 30° of knee flexion, axial, and Merchant views, should be conducted. If there is suspicion of malalignment, a leg-length film should also be included. Merchant views allow for the evaluation of patellar tilt, patellar subluxation, and trochlear dysplasia [24]. Patellar subluxation can be measured using the congruence angle, with an average of 6° ± 11° in the medial direction. Trochlear dysplasia should be considered when the sulcus angle, with an average of 138° ± 6°, is greater than 145°. In lateral radiographs, various methods such as Blackburne-Peel ratio, Koshino ratio, Insall-Salvati ratio, and Caton-Deschamps index (CDI) are employed to assess patellar height.
Magnetic resonance imaging (MRI) is beneficial in evaluating soft-tissue damage and the condition of structures such as the MPFL. It proves useful in identifying osteochondral injuries and loose bodies after traumatic dislocations. In addition to these applications, MRI provides more detailed morphological information to classify at-risk patients and aid in treatment planning.
Computed tomography (CT) enables the measurement of the TT-TG distance by obtaining projections of axial sections passing through the levels of the tibial tubercle and trochlear groove. A distance greater than 20 millimeters (mm) has been demonstrated to be associated with patellar instability [25].
5. Treatment
The majority of studies addressing the treatment of initial patellar dislocation focus on preventing recurrence and addressing associated injuries. Limited attention has been given to preventing short-term symptoms like anterior knee pain or long-term consequences such as the development of patellofemoral osteoarthritis. Various conservative and surgical treatment methods are employed in the management of patellar dislocation. The diversity in treatment approaches stems from the potential inadequacy of treatments due to underlying additional pathologies associated with patellar instability. In order to assist in making treatment decisions, treatment algorithms depicted in Figure 1 can be utilized. Given the diverse ways in which patellar instability can manifest, there may be situations that fall outside the scope of these algorithms.
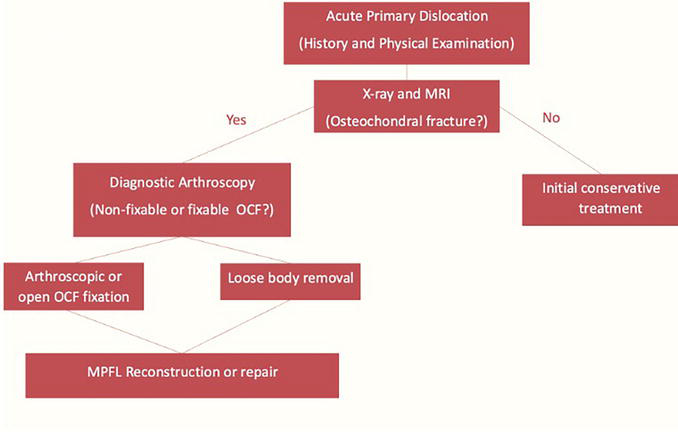
Figure 1.
Treatment algorithm of acute primary patellar dislocation.
5.1 Conservative treatment
In cases of first-time patellar dislocation, conservative treatment is employed as the initial approach, unless there is an associated osteochondral fragment (≥5 mm), bony avulsion of the MPFL, or meniscal tear [26]. This approach has been collectively recommended by the International Patellofemoral Study Group [27]. However, Magnussen et al. reported that only 26.4% of patients treated conservatively returned to their preinjury activity levels, on average, 3 years later [5]. Pagliazzi et al., in a meta-analysis, found no significant difference in long-term Kujala scores between surgically and conservatively treated patients [2]. According to a high-level evidence study, there is a high likelihood of spontaneous healing, and conservative treatment may be applied, especially if the MPFL rupture occurs in the region where the fibers of the vastus medialis obliquus overlap with the MPFL fibers [28].
Following an acute dislocation, the primary objectives are to reduce swelling and pain, strengthen the vastus medialis and gluteal muscles, and regain knee mobility. Rehabilitation protocols vary significantly based on the duration of immobilization and individual needs following the initial dislocation. While some authors recommend immediate mobilization, others suggest immobilization with a cast or brace for up to 6 weeks [29]. Nonetheless, there is a lack of clear evidence supporting the immobilization of the knee after patellar dislocation [9]. Additionally, there is no consensus on the specific duration of knee immobilization, which generally varies from 0 to 6 weeks, and the degree of motion permitted by bracing [30, 31]. Divergent recommendations include maintaining an extension position, starting from 30° of flexion and progressing to 90° after several weeks. Consequently, the type of knee brace may also vary among different studies [32, 33]. Maenpaa et al. found no significant differences in functional outcomes between immediate mobilization and flexion restriction in their study of 72 patients treated conservatively following a first patellar dislocation [34].
Physical therapy and rehabilitation experts agree that kinesiotherapy is essential for achieving full joint range of motion, and quad-strengthening exercises are believed to restore the dynamic component of patellar soft-tissue stabilizers [35]. The average reported time for patients to return to their previous occupations and resume sports activities is around three months [32]. Following the first patellar dislocation, clinical outcomes, functional results, and recurrence rates vary between 36.4% and 73% [3, 35].
5.2 Operative treatment
Patients who require surgical intervention without delay following the first patellar dislocation are those with patellar subluxation or dislocation resulting from the disruption of medial stabilizing structures, accompanied by intra-articular osteochondral fragments or significant cartilage damage (Figures 2 and 3) [36]. In the surgical treatment of patellar dislocation, repair or reconstruction of the MPFL can be performed. Following medial patellofemoral ligament repair, patients can return to their preinjury activity levels; however, the risk of recurrent patellar dislocation is higher compared to MPFL reconstruction [9]. Additionally, isolated MPFL reconstruction has been shown to be indicated in recurrent patellofemoral dislocations without malalignment, trochlear dysplasia, and patella alta. However, MPFL reconstruction alone should not be performed in the presence of risk factors; rather, treatment should be tailored to address these risk factors [37]. Patients with instability symptoms, osteochondral fractures, and those who have failed conservative treatment are recommended to undergo MPFL reconstruction even in the absence of recurrent patellar dislocation [36].
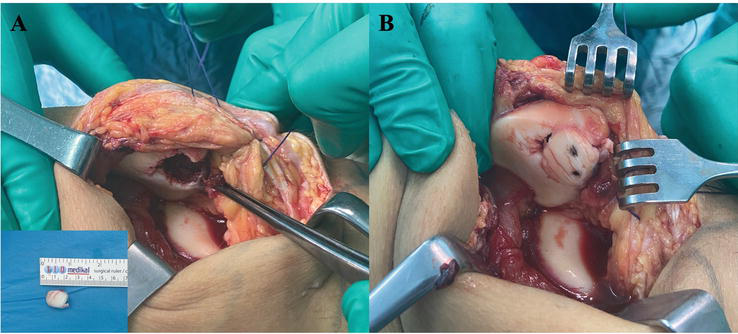
Figure 2.
Osteochondral fracture occurs after primary patellar dislocation (A) and fixation of the fracture with headless screws (B).
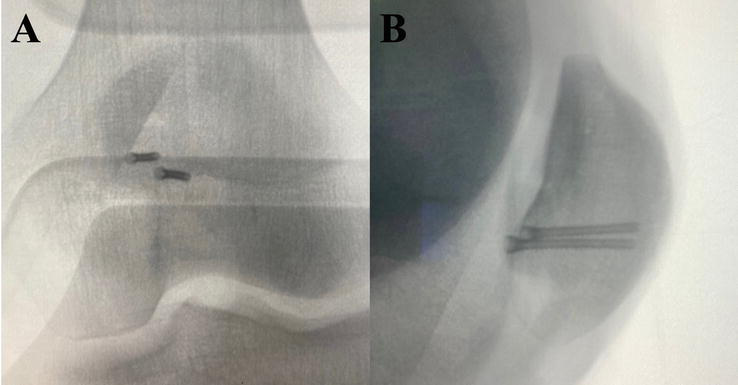
Figure 3.
Intraoperative anteroposterior (A) and lateral (B) fluoroscopy image.
5.2.1 MPFL repair
Certain authors advocate for the rule of repairing the MPFL after the initial patellar dislocation [38]. MPFL repair is considered if the lesion’s location is identified, typically within three weeks of the trauma. Specifically, an MPFL injury at the patellar origin can be addressed through repair. Patellar MPFL lesions can be categorized as ligamentous or bony avulsions, or they may be associated with an osteochondral fragment with involvement of the articular cartilage.
Advocates of this approach assert that repairing the MPFL at its patellar origin facilitates the restoration of the ligament’s anatomical position, avoiding complications and ensuring proper tension of the ligament. Literature reports indicate a redislocation rate following arthroscopic medial retinacular repair/plication, employing similar techniques, ranging from 0 to 19% [39]. Christiansen et al. reported a 17% redislocation rate in the operative group and 20% in the conservative group. The Kujala score was higher in the operative group compared to the conservative group, with significantly improved patella stability in the operative cohort [40]. Some authors suggest that both MPFL repair and reconstruction are effective in restoring preinjury activity levels. However, the failure rate, defined as recurrent patellar instability, tends to be higher with MPFL repair when compared to MPFL reconstruction [41].
5.2.2 MPFL reconstruction
Currently, the primary approach for proximal soft-tissue stabilization procedures is MPFL reconstruction, which significantly decreases subjective instability and occurrences of frank dislocations. Research has indicated that the MPFL is frequently injured at various points along its length [10]. This complexity can pose challenges in accurately identifying the torn segments of the MPFL, both through imaging and during surgical procedures, potentially resulting in unsuccessful repairs. MPFL reconstruction is utilized 1.5 times more frequently than repair or medial retinacular/plication. It seems to offer more consistent results following the initial patellar dislocation, encompassing both clinical outcomes and the redislocation rate [42].
In the case of the initial dislocation, indications for MPFL reconstruction include the presence of an osteochondral fracture or the persistence of symptoms after conservative treatment. One of the most common indications for medial patellofemoral ligament reconstruction is a history of recurrent lateral patellar dislocation. The systematic review indicates that surgical treatment reduces the rates of recurrent instability, increases participation in sports, and improves the quality of life [43]. Various methods have been described for MPFL reconstruction. The commonality among all these methods is the creation of a new ligament extending from the patella to the femur. The most commonly used techniques for MPFL reconstruction involve procedures using hamstring tendons. Autografts obtained from the hamstrings are utilized to complete the reconstruction by fixing them in tunnels or sockets created in the patella, with the aid of tenodesis screws or suture anchors, forming a double-bundle reconstruction. The tunnels created can pass entirely through the patella in the medial-lateral plane or, alternatively, half tunnels can be formed, leaving the lateral cortex intact. A prospective study conducted by Ercan et al. demonstrated no clinical, radiological, or functional differences between single-tunnel and double-tunnel MPFL reconstructions [44].
Xie et al. reported a substantial and statistically significant increase in Tegner’s score with MPFL reconstruction using the semitendinosus tendon graft in 85 knees. Additionally, they documented a redislocation rate of 1.1% [45]. In a comprehensive review of 25 papers discussing diverse surgical approaches for addressing the initial patellar dislocation, which included additional bone procedures, Shah et al. reported a reduced redislocation rate (3.7%) among patients undergoing MPFL reconstruction [46].
5.3 Surgical versus conservative treatment
The selection between surgical and conservative treatment after the initial patellar dislocation is not clearly defined, and patient selection plays a crucial role. The recurrence rates of dislocation vary in both groups. It is believed that recurrent dislocations are associated with a young age and a high level of activity [47]. Longo et al. have shown that the risk of recurrence is lower in those who undergo surgical treatment after the initial patellar dislocation [3]. Smith et al. conducted a study demonstrating that surgical treatment reduces the risk of recurrent dislocation but increases the risk of patellofemoral osteoarthritis. This situation may be related to changes in knee kinematics [48]. In a study with a 14-year follow-up conducted by Palmu et al., it was shown that patients treated conservatively and surgically had similar rates of recurrent dislocation [33]. In a meta-analysis conducted by Migliorini et al. in 2020, patients treated surgically and conservatively after the initial patellar dislocation were compared. It was reported that surgically treated patients showed a significant increase in Kujala knee scores and a decrease in the risk of persistent joint instability and recurrent dislocation. Better outcomes were found in patients who underwent surgical treatment during the 30- and 60-month follow-ups [49].
After the first patellar dislocation, individuals under the age of 16, those with contralateral instability, trochlear dysplasia, patella alta, TT-TG distance greater than 16 mm, and patellar tilt exceeding 20° are at significantly increased risk of recurrent patellar instability if they have four or more of these conditions. Surgical intervention is anticipated to be beneficial for these patients [50]. It has been suggested that bone deformities following the initial patellar dislocation may not necessarily be treated, especially if not addressed after the first dislocation [51]. However, when a second patellar dislocation occurs, particularly in adults, trochlear dysplasia or malalignment should be addressed. Sillanpaa et al. have stated that intervention on the bone may not be necessary after the first patellar dislocation but becomes essential for achieving proper bone alignment in cases with severe anomalies [9]. As the degree of trochlear dysplasia increases, the risk of recurrent patellar dislocation also rises [52]. In patients with severe anatomical patellofemoral deformities, trochlear dysplasia, or an elongated TT-TG distance, tibial tubercle transposition or trochleoplasty should be considered in conjunction with MPFL repair/reconstruction [51]. Isolated MPFL reconstruction has also been reported to yield good results in the presence of trochlear dysplasia in the literature [37]. Patellofemoral joint osteoarthritis constitutes a relative contraindication for MPFL reconstruction. This is because restricting the patella results in significant reactive forces in the joint, accelerates osteoarthritis, and worsens pain [53].
Many studies do not provide clear answers regarding the choice between conservative and surgical treatment after the initial patellar dislocation [9]; deciding which treatment will benefit which patient requires considering the risk-benefit ratio. Conservative treatment offers advantages such as a faster return to work and sports with lower costs and without surgical risks [54]; however, the risk of cartilage and ligament damage increases with conservative treatment. Additionally, the functional outcomes, level of quality of life, and time to return to sports are not clearly defined. In surgical treatment, the return period may be longer, and there are surgical complications such as infection and joint movement limitation. It is unknown whether surgical treatment is chondroprotective, and the functional outcomes, level of quality of life, and time to return to sports are not clearly known [54].
While many aspects of treatment remain controversial, some issues have gained clarity. Not all patellar dislocations are the same, and not every patient tolerates conservative treatment well. Understanding the risk factors is important in predicting and managing patients who may develop recurrent patellofemoral instability [54, 55]. Although it may not be clear which patients should undergo conservative or surgical treatment after the initial dislocation, it can be predicted that patients with major and minor risk factors may benefit from surgical treatment. However, when deciding on surgery, the condition of the cartilage, soft-tissue balance, potential osteochondral damage, and the risk of osteoarthritis should also be considered.
6. Conclusion
Although conservative treatment is recommended for acute first traumatic dislocation today, making definitive conclusions is not possible due to the limitations in sample size and randomization in the studies in the literature. Surgical treatment is recommended in the presence of accompanying osteochondral fractures. Repairing a torn MPFL may be considered, especially in cases of (bony) avulsion from the patella. However, it has been demonstrated that MPFL reconstruction is more reliable than repair. Importantly, there is no evidence supporting the necessity to correct bone abnormalities following the initial episode of patellar dislocation. While early surgical intervention has been shown to yield better results in terms of recurrent instability and functional scoring, no significant difference from conservative treatment has been demonstrated in the late period. Randomized controlled trials assessing the impact of facilitating factors on outcomes may provide guidance in the future.
References
- 1.
Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA, et al. Epidemiology and natural history of acute patellar dislocation. The American Journal of Sports Medicine. 2004; 32 (5):1114-1121 - 2.
Pagliazzi G, Napoli F, Previtali D, Filardo G, Zaffagnini S, Candrian C. A meta-analysis of surgical versus nonsurgical treatment of primary patella dislocation. Arthroscopy. 2019; 35 (8):2469-2481 - 3.
Longo UG, Ciuffreda M, Locher J, Berton A, Salvatore G, Denaro V. Treatment of primary acute patellar dislocation: Systematic review and quantitative synthesis of the literature. Clinical Journal of Sport Medicine. 2017; 27 (6):511-523 - 4.
Sillanpää P, Mattila VM, Iivonen T, Visuri T, Pihlajamäki H. Incidence and risk factors of acute traumatic primary patellar dislocation. Medicine and Science in Sports and Exercise. 2008; 40 (4):606-611 - 5.
Magnussen RA, Verlage M, Stock E, et al. Primary patellar dislocations without surgical stabilization or recurrence: How well are these patients really doing? Knee Surgery, Sports Traumatology, Arthroscopy. 2017; 25 (8):2352-2356 - 6.
Duthon VB. Acute traumatic patellar dislocation. Orthopaedics & Traumatology, Surgery & Research. 2015; 101 (1 Suppl):S59-S67 - 7.
Nomura E, Inoue M, Kurimura M. Chondral and osteochondral injuries associated with acute patellar dislocation. Arthroscopy. 2003; 19 (7):717-721 - 8.
Panni AS, Cerciello S, Vasso M. Patellofemoral instability: Surgical treatment of soft tissues. Joints. 2013; 1 (1):34-39 - 9.
Sillanpää PJ, Mäenpää HM. First-time patellar dislocation: Surgery or conservative treatment? Sports Medicine and Arthroscopy Review. 2012; 20 (3):128-135 - 10.
Weber-Spickschen TS, Spang J, Kohn L, Imhoff AB, Schottle PB. The relationship between trochlear dysplasia and medial patellofemoral ligament rupture location after patellar dislocation: An MRI evaluation. The Knee. 2011; 18 (3):185-188 - 11.
Petri M, Ettinger M, Stuebig T, et al. Current concepts for patellar dislocation. Archives of Trauma Research. 2015; 4 (3):e29301 - 12.
Johnson DS, Turner PG. Management of the first-time lateral patellar dislocation. The Knee. 2019; 26 (6):1161-1165 - 13.
Cash JD, Hughston JC. Treatment of acute patellar dislocation. The American Journal of Sports Medicine. 1988; 16 (3):244-249 - 14.
LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L. The anatomy of the medial part of the knee. The Journal of Bone and Joint Surgery. American Volume. 2007; 89 (9):2000-2010 - 15.
Stephen JM, Lumpaopong P, Deehan DJ, Kader D, Amis AA. The medial patellofemoral ligament: Location of femoral attachment and length change patterns resulting from anatomic and nonanatomic attachments. The American Journal of Sports Medicine. 2012; 40 (8):1871-1879 - 16.
Lewallen L, McIntosh A, Dahm D. First-time patellofemoral dislocation: Risk factors for recurrent instability. The Journal of Knee Surgery. 2015; 28 (4):303-309 - 17.
Steensen RN, Bentley JC, Trinh TQ , Backes JR, Wiltfong RE. The prevalence and combined prevalences of anatomic factors associated with recurrent patellar dislocation: A magnetic resonance imaging study. The American Journal of Sports Medicine. 2015; 43 (4):921-927 - 18.
Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. The American Journal of Sports Medicine. 2000; 28 (4):472-479 - 19.
Bassett FH. Acute dislocation of the patella, osteochondral fractures, and injuries to the extensor mechanism of the knee. Instructional Course Lectures. 1976; 25 :40-49 - 20.
Dimon JH 3rd. Apprehension test for subluxation of the patella. Clinical Orthopaedics and Related Research. 1974; 103 :39 - 21.
Skalley TC, Terry GC, Teitge RA. The quantitative measurement of normal passive medial and lateral patellar motion limits. The American Journal of Sports Medicine. 1993; 21 (5):728-732 - 22.
Boden BP, Pearsall AW, Garrett WE Jr, Feagin JA Jr. Patellofemoral instability: Evaluation and management. The Journal of the American Academy of Orthopaedic Surgeons. 1997; 5 (1):47-57 - 23.
Post WR. Clinical evaluation of patients with patellofemoral disorders. Arthroscopy. 1999; 15 (8):841-851 - 24.
Wolfe S, Varacallo M, Thomas JD, Carroll JJ, Kahwaji CI. Patellar instability. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023 - 25.
Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: An anatomic radiographic study. Knee Surgery, Sports Traumatology, Arthroscopy. 1994; 2 (1):19-26 - 26.
Duerr RA, Chauhan A, Frank DA, DeMeo PJ, Akhavan S. An algorithm for diagnosing and treating primary and recurrent patellar instability. JBJS Reviews. 2016; 4 (9):e2 - 27.
Liu JN, Steinhaus ME, Kalbian IL, et al. Patellar instability management: A survey of the international patellofemoral study group. The American Journal of Sports Medicine. 2018; 46 (13):3299-3306 - 28.
Servien E, Fritsch B, Lustig S, et al. In vivo positioning analysis of medial patellofemoral ligament reconstruction. The American Journal of Sports Medicine. 2011; 39 (1):134-139 - 29.
Dixit S, Deu RS. Nonoperative treatment of patellar instability. Sports Medicine and Arthroscopy Review. 2017; 25 (2):72-77 - 30.
Apostolovic M, Vukomanovic B, Slavkovic N, et al. Acute patellar dislocation in adolescents: Operative versus nonoperative treatment. International Orthopaedics. 2011; 35 (10):1483-1487 - 31.
Sillanpää PJ, Mattila VM, Mäenpää H, Kiuru M, Visuri T, Pihlajamäki H. Treatment with and without initial stabilizing surgery for primary traumatic patellar dislocation. A prospective randomized study. The Journal of Bone and Joint Surgery. American Volume. 2009; 91 (2):263-273 - 32.
Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y. Acute patellar dislocation in children and adolescents: A randomized clinical trial. The Journal of Bone and Joint Surgery. American Volume. 2008; 90 (3):463-470 - 33.
Regalado G, Lintula H, Kokki H, Kröger H, Väätäinen U, Eskelinen M. Six-year outcome after non-surgical versus surgical treatment of acute primary patellar dislocation in adolescents: A prospective randomized trial. Knee Surgery, Sports Traumatology, Arthroscopy. 2016; 24 (1):6-11 - 34.
Maenpaa H, Sillanpaa PJ, Paakkala A. A prospective, randomized trial following conservative treatment in acute primary patellar dislocation with special reference to patellar braces. Knee Surgery, Sports Traumatology, Arthroscopy. 2010; 18 (Suppl 1):119 - 35.
Smith TO, Davies L, Chester R, Clark A, Donell ST. Clinical outcomes of rehabilitation for patients following lateral patellar dislocation: A systematic review. Physiotherapy. 2010; 96 (4):269-281 - 36.
Dall'Oca C, Elena N, Lunardelli E, Ulgelmo M, Magnan B. MPFL reconstruction: Indications and results. Acta Bio-Medica. 2020; 91 (4-S):128-135 - 37.
Petri M, von Falck C, Broese M, et al. Influence of rupture patterns of the medial patellofemoral ligament (MPFL) on the outcome after operative treatment of traumatic patellar dislocation. Knee Surgery, Sports Traumatology, Arthroscopy. 2013; 21 (3):683-689 - 38.
Mariani PP, Liguori L, Cerullo G, Iannella G, Floris L. Arthroscopic patellar reinsertion of the MPFL in acute patellar dislocations. Knee Surgery, Sports Traumatology, Arthroscopy. 2011; 19 (4):628-633 - 39.
Sillanpää PJ, Mäenpää HM, Mattila VM, Visuri T, Pihlajamäki H. Arthroscopic surgery for primary traumatic patellar dislocation: A prospective, nonrandomized study comparing patients treated with and without acute arthroscopic stabilization with a median 7-year follow-up. The American Journal of Sports Medicine. 2008; 36 (12):2301-2309 - 40.
Christiansen SE, Jakobsen BW, Lund B, Lind M. Isolated repair of the medial patellofemoral ligament in primary dislocation of the patella: A prospective randomized study. Arthroscopy. 2008; 24 (8):881-887 - 41.
Matic GT, Magnussen RA, Kolovich GP, Flanigan DC. Return to activity after medial patellofemoral ligament repair or reconstruction. Arthroscopy. 2014; 30 (8):1018-1025 - 42.
Smith TO, Walker J, Russell N. Outcomes of medial patellofemoral ligament reconstruction for patellar instability: A systematic review. Knee Surgery, Sports Traumatology, Arthroscopy. 2007; 15 (11):1301-1314 - 43.
Nwachukwu BU, So C, Schairer WW, Green DW, Dodwell ER. Surgical versus conservative management of acute patellar dislocation in children and adolescents: A systematic review. Knee Surgery, Sports Traumatology, Arthroscopy. 2016; 24 (3):760-767 - 44.
Ercan N, Akmese R, Ulusoy B. Single-tunnel and double-tunnel medial patellofemoral ligament reconstructions have similar clinical, radiological and functional results. Knee Surgery, Sports Traumatology, Arthroscopy. 2021; 29 (6):1904-1912 - 45.
Xie G, Zhao J, Huangfu X, He Y. Medial patellofemoral ligament reconstruction using semitendinosus tendons: Polyester suture augmentation versus nonaugmentation. The American Journal of Sports Medicine. 2012; 40 (6):1365-1374 - 46.
Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. The American Journal of Sports Medicine. 2012; 40 (8):1916-1923 - 47.
Kang HJ, Wang F, Chen BC, Zhang YZ, Ma L. Non-surgical treatment for acute patellar dislocation with special emphasis on the MPFL injury patterns. Knee Surgery, Sports Traumatology, Arthroscopy. 2013; 21 (2):325-331 - 48.
Smith TO, Song F, Donell ST, Hing CB. Operative versus non-operative management of patellar dislocation. A meta-analysis. Knee Surgery, Sports Traumatology, Arthroscopy. 2011; 19 (6):988-998 - 49.
Migliorini F, Driessen A, Quack V, Gatz M, Tingart M, Eschweiler J. Surgical versus conservative treatment for first patellofemoral dislocations: A meta-analysis of clinical trials. European Journal of Orthopaedic Surgery and Traumatology. 2020; 30 (5):771-780 - 50.
Parikh SN, Lykissas MG, Gkiatas I. Predicting risk of recurrent patellar dislocation. Current Reviews in Musculoskeletal Medicine. 2018; 11 (2):253-260 - 51.
Bulgheroni E, Vasso M, Losco M, et al. Management of the first patellar dislocation: A narrative review. Joints. 2019; 7 (3):107-114 - 52.
Melegari TM, Parks BG, Matthews LS. Patellofemoral contact area and pressure after medial patellofemoral ligament reconstruction. The American Journal of Sports Medicine. 2008; 36 (4):747-752 - 53.
Purohit N, Hancock N, Saifuddin A. Surgical management of patellofemoral instability part 2: Post-operative imaging. Skeletal Radiology. 2019; 48 (7):1001-1009 - 54.
Rund JM, Hinckel BB, Sherman SL. Acute patellofemoral dislocation: Controversial decision-making. Current Reviews in Musculoskeletal Medicine. 2021; 14 (1):82-87 - 55.
Huntington LS, Webster KE, Devitt BM, Scanlon JP, Feller JA. Factors associated with an increased risk of recurrence after a first-time patellar dislocation: A systematic review and meta-analysis. The American Journal of Sports Medicine. 2020; 48 (10):2552-2562