Clinical characteristics of complete III nerve palsy.
Abstract
Paralytic strabismus is caused by paresis or paralysis of one or more extraocular muscles that are innervated by cranial nerve lll, IV and Vl. They are characterized by squinting angle that depends on the direction of the gaze and the fixating eye. Typically, the angle is greater in the field of affected muscle, and when the patient is fixing with the affected eye. While younger children in some cases can suppress double vision, older children and adults with acquired paralytic strabismus usually have diplopia, which they try to avoid by compensatory head posture. Some types of paralytic strabismus can be congenital but it is important to diagnose acquired paralytic strabismus that can be caused by some neurological or systemic disorders and requires further investigation. Treatment of the paralytic strabismus is challenging, and despite the multiple surgeries, results can be disappointing.
Keywords
- paralytic strabismus
- third nerve palsy
- sixth nerve palsy
- fourth nerve palsy
- eye muscle surgeries
1. Introduction
Paralytic strabismus is caused by paresis or paralysis of one or more extraocular muscles. They are characterised by incomitant strabismus with the variable squinting angle that depends on the direction of the gaze and the fixating eye. Typically, the angle is greater in the field of affected muscle, and when the patient is fixing with the affected eye. While younger children can suppress double vision, older children and adults with acquired paralytic strabismus usually have diplopia, which they try to avoid by compensatory head posture (CHP). It is important to distinguish acquired paralytic strabismus from the comitant form. Acquired paralytic form may be caused by some neurological or systemic abnormalities, requires further neurological investigation and can be life threatening. Treatment of paralytic strabismus is challenging, and despite multiple surgeries, results can be disappointing.
2. Third nerve palsy
Oculomotor palsy can be congenital or acquired, complete or partial, pupil-sparing or pupil-involving and isolated or accompanied by neurological conditions [1].
Third nerve palsy in children is usually congenital but can be acquired later as a result of trauma, inflammation or rarely from neoplastic lesions. Congenital palsies are usually secondary to maldevelopment, intrauterine insult or birth trauma. When bilateral, congenital lll nerve palsies are usually a part of congenital cranial dysinnervation disorders (CCDD) in which genetic mutations lead to abnormal development of cranial nerves III, IV and VI, which results in secondary changes of extraocular muscles and development of a complex, incomitant strabismus. Unilateral cases may be a part of neurofibromatosis type II, posterior fossa malformations, septo-optic dysplasia or some other neurological disorders [2]. Among acquired forms, trauma is the most common cause in child’s age, trauma and infections together with aneurysms, diabetes or microvascular infarction are more often cause of third nerve palsy in adults. Children can have transient ophthalmoplegia following infection or migraine [3]. The clinical picture should be always correlated with the age and systemic diseases of the patient.
The nuclear complex of oculomotorius nerve lies in the midbrain and each muscle has its own subnucleus [4].
2.1 Subnuclei of III nerve
Clinical picture can be different depending on which part of the III nerve is involved. In cases of total palsy, position of the affected eye is typically ‘down and out’, determined by the function of two intact muscles, the lateral rectus and superior oblique muscle. Affected eye will be in abduction, with slight depression and intorsion with ptosis of affected lid and dilated pupil unreactive to light and accommodation (Figure 1). Movement deficit will include adduction, elevation and depression with motility possible only in abduction and to small degree in depression with incyclotorsion (action of the superior oblique, which is minor when eye is abducted). Due to relaxation in tonus of four extraocular muscles, a small amount of proptosis can be present. Adult patients or older children will experience diplopia, which can be horizontal, vertical or oblique, depending on the muscle involved. Younger children due to cortical suppression of the image of the deviated eye may not develop double vision. In cases of longstanding palsy, or palsy that is progressing gradually over time, development of aberrant nerve regeneration can take place, which leads sometimes to perplexing clinical picture. Most often misdirection is presented as anomalous lid excursion during the movement of the eye (retraction of the lid during the movement of the eye), or abnormal horizontal or vertical movement during the attempt to move the eye in the field of action of the affected muscle. Table 1 shows clinical characteristics of complete III nerve palsy.

Figure 1.
Clinical picture of bilateral III nerve palsy.
| Clinical characterisitcs of the complete III nerve palsy |
|---|
| Eye “out and down”, large exotropia with a small hypotropia, intorsion |
| Ptosis |
| Fixed and dilated pupil |
| Reduced: adduction, elevation and depression |
| Motility: abduction, small amount of depression and incyclotorsion |
| Compensatory head posture: face turned to the opposite side and chin up |
Table 1.
In cases of partial involvement, any combination of the affected muscles and/or lid and pupil can be involved. Superior division (superior rectus muscle and levator palpebre) or inferior division (rectus superior and medialis, and inferior oblique muscle) can be affected independently. Each of individual muscles can be involved alone or in combination with each other.
After diagnosing the palsy on the basis of clinical picture and history, it is obligatory to continue the investigation of the aetiology. Neurological examination together with imaging (CT and/or MRI) are usually required. In some congenital cases, where diagnosis of palsy is clearly not connected with some progressive neurologic or systemic disease, imaging is not obligatory. Acquired III nerve palsy in children is usually sign of some underlying neurological disease. Associated neurological or systemic signs and symptoms will help examiner to clear etiology of the palsy. The need for repeated imaging is controversial; some suggest that in cases of unclear aetiology, imaging should be repeated after one or two years to exclude some neoplastic or vascular abnormality that was too subtle to be found during the first imaging.
2.2 Differential diagnosis
The diagnosis in the III nerve palsy is usually clear in the cases of complete muscle paresis but can be perplexing in partial palsies when different muscles are involved. Myasthenia gravis or multiple sclerosis can mimic clinical picture of III nerve palsy with lid involvement. Double elevator palsy or orbital floor fracture can have similar clinical picture as superior division palsy.
2.3 Treatment
At child’s age, risk of developing amblyopia is high and has to be treated with conservative treatment aggressively and immediately from the beginning, with refractive correction and patching. In congenital cases with no chances for recovery, surgery has to be planned at an early age. In cases of acquired palsy, chances of spontaneous recovery are sometimes good, so surgery should be postponed for at least 6 months. Conservative treatment is based on alleviating double vision with prism correction when possible, or occlusion of the affected eye. Surgery is the method of choice in the cases of acquired, non-progressive palsy that does not improve or resolve during the period of 6–12 months. Surgical approach depends on the muscle involved and extent of the paresis (complete or partial). In cases of complete palsy, often more than one surgery is required with the result that is only partially satisfying in appearance and functionality. In some cases, in early stages, botulinum toxin can be helpful. It is obligatory to talk to the patient before the surgery and explain that operation will not enable normal movement of the eye, but only restore usable field of binocular single vision and achieve acceptable appearance. The type of surgery can vary depending on the muscles involved and amount of action that is present in the affected muscle. Varying from combined recess-resect procedures in supramaximal numbers up to 15 mm. Although in the beginning, results of the surgery are satisfactory the effect of the surgery diminishes over time. Vertical deviation can be improved during the combined horizontal procedure with vertical transposition of horizontal muscles or by performing recession and resection of vertical muscles. Transposition surgeries on SO can be performed in more complicated cases with complete third nerve palsies [5]. Aberrant regeneration improves strabismic deviation but may be complicated to solve during surgical interventions.
Ptosis surgery has to be considered after the strabismus surgeries are completed. The type of intervention depends on levator muscle function (levator resection or frontalis sling surgery) with care taken about the corneal exposure.
3. Sixth nerve palsy
Palsies of the sixth nerve are less common in children but are most often palsies of cranial nerves in adult patients [6]. Typical clinical picture is characterised as an esotropia in primary position (Figure 2) with increasing deviation in the field of paretic lateral rectus. The nucleus of nervus abducens is situated in caudal part of pons and innervates lateral rectus muscle on the same side. Fibres of cranial nerve VII loop around the sixth nerve nucleus, therefore, lesions of these two nerves can often occur together.

Figure 2.
Clinical picture of VI nerve palsy before and after surgery, (medial rectus recession + Hummelsheim procedure).
Children with sixth nerve palsy can develop and preserve binocular vision by adopting compensatory head postures by turning the head in the direction of the affected muscle. Deviation is bigger at distance than near. Congenital sixth nerve palsy in children is rare; however, transient lateral rectus palsy can be present in newborns with spontaneous resolution within 6 weeks. Apart from neurological causes (brain stem pathology, hydrocephalus) or trauma, common cause of ‘benign’ acquired palsy in early childhood can be isolated sixth nerve palsy related to infectious or immunological process. This kind of postviral inflammatory neuropathy typically has an acute onset 1–3 weeks after viral infection or immunisation [8]. These children have to be closely monitored during the improvement, which usually takes 3–6 months. Although recurrences can happen in this kind of palsy, in cases of multiple recurrences or incomplete recovery, additional neurological work up and imaging are recommended to exclude other causes (occult tumour) [9]. In some cases of elevated intracranial pressure, meningitis or excessive trauma sixth nerve palsy can be bilateral. In adult patients, microvascular diseases (diabetes, hypertension or atherosclerosis) together with closed-head trauma are among leading causes. Clinical characteristics of sixth nerve palsy are shown in Table 2.
| Clinical characterisitcs of VI nerve palsy |
|---|
| Reduction of abduction on affected eye |
| Deviation greater at distance than at near |
| Deviation greater when affected eye is fixing |
| In unilateral or cases with asymmetry: head turn towards affected side |
| Esotropia that increases when looking to the affected side |
Table 2.
Clinical characteristics of VI nerve palsy.
3.1 Differential diagnosis
In newborns, early esotropia syndrome can be misdiagnosed as a congenital sixth nerve palsy. The difference between these two disorders can be made by demonstrating full abduction of the affected eye by doll’s head manoeuvre. Duane retraction sy or Mobius sy have impaired abduction but these disorders are presented with restriction rather than limitation, which is manifested by retraction of the globe, narrowing of the lid aperture and an upshot and downshoot in adduction [7].
3.2 Treatment
Conservative treatment includes prevention of amblyopia in child’s age. Care should be taken, especially in children who do not turn their heads, because that can indicate suppression of the deviated eye and lead to amblyopia. Refractive error has to be corrected together with patching of unaffected eye. Majority of cases of acquired abducens palsy will recover during the period of six months. In cases when spontaneous recovery does not occur, surgery is indicated. Surgery depends on amount of action that is present in the affected muscle [10]. In cases of partial palsy when some of the functions are still possible, combined, graded surgery in augmented numbers (recess/resect with calculations based on preserved function) on both horizontal rectus muscles is usually performed. In the cases of complete palsy with no remained function, muscle transposition surgeries are usually method of choice. The full tendon transposition of vertical muscles towards lateral rectus is not a method of choice avoiding the risk of anterior segment ischemia. Therefore, other, more vessel-sparing procedures are commonly used (Hummelsheim, Jensen and different kinds of modifications). In

Figure 3.
Hummelsheim procedure.
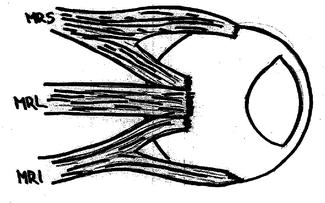
Figure 4.
Jensen procedure.
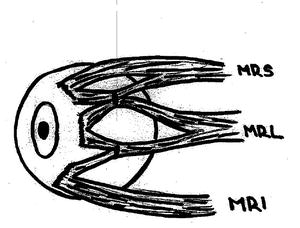
Figure 5.
Nishida procedure.
4. Fourth nerve palsy
Fourth cranial nerve innervates superior oblique muscle. Palsy can be congenital or acquired. Although the term unilateral congenital fourth nerve palsy is widely used in the cases of elevation in adduction in children, some clinical characteristics strongly suggest that not all of the cases with elevation in adduction are fourth nerve palsy. Differences should be noticed between the cases of true palsy where typical signs of paresis, such as increasing deviation in the field of affected muscle, are present, and cases of inferior oblique overaction (IOOA) where the deviation is same in different gaze directions (no incomitance). In non-paretic cases, the deviation should be classified as IOOA or strabismus sursoaductorius (Figure 6). In the cases of IOOA despite marked vertical deviation, patients do not complain of diplopia except in the cases of decompensation. However, in some congenital cases, signs of incomitance are present or/and signs of muscle absence or not fully developed superior oblique muscle are found on imaging. Therefore, these cases are truly congenital cases of superior oblique muscle palsy. Clinical differences between IOOA and congenital fourth nerve palsy are presented in Table 3. The distinction between congenital and acquired palsy is important because recently diagnosed palsy can be result of intracranial lesion and requires neurologic investigation [11].
| Clinical features | IOOA (or strabismus sursoaductorius) | Trochlear palsy |
|---|---|---|
| History (old photo) | Head tilt or turn | Negative |
| Onset | Intermittent | Sudden |
| Vertical deviaton | Comitant in adduction | Maximum in down gaze |
| Cyclotropic deviation | Small, comittant | Maximum in down gaze |
| Elevation in adduction | Marked | Negative |
| Vertical fusional amplitude | Enlarged (up to 15 PD) | Normal (2-3 PD) |
| Beilschowsky head tilt test | Same in up, pp and down gaze | Maximum in down gaze |
| Facial asymmetry | Fuller face of the affected side | Negative |
Table 3.
Differences in clinical picture between strabismus sursoaductorius (IOOA) and unilateral acquired fourth nerve palsy.
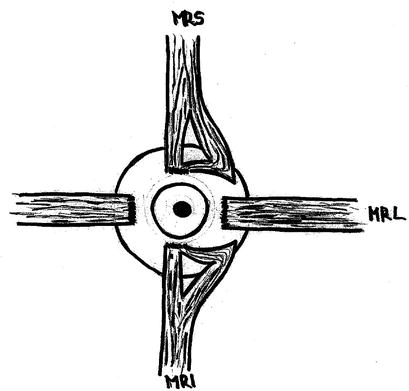
Figure 6.
Differences in clinical picture between fourth nerve palsy and IOOA (CHP).
Acquired cases are more common in adults. Most common causes are closed-head trauma, vascular lesions and intracranial tumours. In cases of traumatic origin, paralysis is often bilateral but asymmetrical. The main clinical sign is excyclotropia, which increases in downgaze. Motility testing reveals under action of affected superior oblique muscle and in some cases, overaction of inferior oblique muscle. Vertical deviation has to be measured in pp, up and down gaze, with amount of deviation larger when eyes are in infraversion. In bilateral cases, V pattern is present. The amount of cyclotorsion is large and increases in downgaze. It can be measured with Madox rod test. However, for measurement of cyclotorsion, as well as vertical and horizontal deviation in the field of 25°–30° of primary positions, the Harms Tangent screen has to be used whenever possible. Torsion can be confirmed by fundus photography. Vertical and torsional double vision are usually present and increasing in the field of action of the affected muscle. In unilateral cases, compensatory head posture is head tilt on other shoulder, sometimes with chin down (Figure 7). Some asymmetric bilateral cases tend to look like unilateral palsy, so care should be taken to confirm if both sides are affected. Bilateral palsies are often in the cases of blunt trauma. When both muscles are affected, patient has marked cyclotropia that is greater in downgaze, with tilted double vision in infraduction and chin up as a compensatory position.

Figure 7.
Harada–Ito procedure.
4.1 Differential diagnosis
Strabismus sursoaductiorius (IOOA) is most common differential diagnosis, especially in congenital cases. In some cases, contralateral superior rectus muscle weakness or DVD on affected eye can have similar clinical symptoms as fourth nerve palsy.
4.2 Treatment
Treatment of underlying disease when possible is first step. In the cases of palsy when underlying disease is not found or not possible to treat, waiting for possible recovery at least six months is recommended. To alleviate torsional double vision, patching of affected eye is often required. Most often complaint that needs correction in patients with acquired fourth nerve palsy is torsion, which can exceed 15° in bilateral cases. Since these deviations cannot be compensated with prism correction, and down gaze is needed functionally in everyday’s activities (reading, eating), surgery is the best method of choice. Surgical treatment depends on the clinical picture. Since excyclotorsion in down gaze is most prominent obstacle to fusion, it has to be addressed first. In the Harada–Ito procedure, anterior part of superior oblique muscle is pulled laterally and anteriorly to the upper border of the lateral rectus (in the direction of muscle action), which is the best choice to correct cyclotorsion. Some modifications of this method (Fells or Boergen modification) are recommended in order to increase the effect on cyclodeviation. Since the anterior part is not detached from the muscle, this kind of surgery will have effect on vertical and horizontal deviation in adduction as well (Figure 7) [12].
In the cases where this kind of surgery is not sufficient, or vertical deviation is more than 5°, additional tuck of posterior part of the superior oblique tendon or combined surgery on oblique muscles can be performed. While this kind of surgery affects predominantly excyclotorsion, which is usually the major problem, especially in bilateral cases, sometimes in monocular cases, when vertical deviation is predominant, transposition of LR and MR downwards can be method of choice.
5. Conclusion
Paralytic eye motility disorders are complex groups of eye motility problems that can be caused by many reasons. Some of the cases are herited, with the possibility to identify the locus that is responsible for the motility impairment, but unfortunately for the time being there is no genetic treatment available. In many cases, motility problems are caused by neurological diseases. Since some neurological diseases can be life-threatening, we have to be well-coordinated with neurologists. Neurological treatment or sometimes neurosurgical treatment can, in some cases, solve problem with eye motility. However, even with help of other specialists and/or conservative ophthalmological treatment, we often have to treat these patients surgically. Surgical approach is often more complex and demanding than treatment in other kinds of strabismus and results are less satisfactory. Surgery has to be the last option, usually after at least six months after the motility problem starts to be sure that possible spontaneous recovery will not take place. In cases of paretic muscles, it is reasonable whenever possible to prefer recessions more than resections to improve mobility. In the cases of total paralysis and good function of other muscles, muscle transposition can also be method of choice. Last but not the least, it is important to talk with patients and try to explain that with surgical treatment, we cannot restore muscle function, but can improve position of the eye, and by that improve double vision and compensatory head position.
References
- 1.
Chugh JP, Prachi J, Chouhan RS, Rathi A. Third nerve palsy: An overview. Indian Journal of Clinical Practice. 2012; 22 (12):17-20 - 2.
Zak R, Slamovits T, Burde R. Oculomotor brainstem anatomy: Nuclei to fascicles. Journal of Neuro-Oncology. 1994; 18 (3):241-248 - 3.
Carlow TJ. Oculomotor ophthalmoplegic migraine: Is it really migraine. Journal of Neuro-Ophthalmology. 2002; 22 (3):215-221 - 4.
Umapathi T, Koon SW, Mukkam RP, Chin LS, Beng TC, Helen T, et al. Insights into three dimensional structure of the oculomotor nuclear complex and fascicles. Journal of Neuro-Ophthalmology. 2000; 20 (2):138-144 - 5.
Simmons BD. Surgical management of ocular motor cranial nere palsyes. Seminars in Ophthalmology. 1999; 1999 :481-494 - 6.
Merino P, de Gomez LP, Villalobo JM, Franco G, de Gmez LR. Etiology and treatmen of pediatric sixth nerve palsy. Journal of AAPOS. 2010; 14 (6):502-505 - 7.
Dotan G, Rosenfeld E, Stolovitch C, Kesler A. The role of neuroimaging in the evaluation process of children with isolated sixth nerve palsy. Childs Nerve System. 2013; 29 (1):89-92 - 8.
Mahoney NR, Liu GT. Benign recurrent sixth (abducens) nerve palsy in children. Archives of Disease in Childhood. 2009; 94 (5):394-396 - 9.
Yuousuf SJ, Khan AO. Presenting features suggestive for later recurrence of idiopathic sixth nerve paresis in children. Journal of AAPOS. 2007; 11 (5):452-455 - 10.
Lyons CJ, Godoy F, ALQahtani E. Surgical management of sixth nerve palsy. Eye. 1987; 1 :78-85 - 11.
Price NC, Vickers S, Lee JP, Fells P. The diagnosis and surgical management of acquired bilateral superior oblique palsy. Eye. 1987; 1 :78-85 - 12.
Ehrt O, Boergen KP. A concept of the surgical treatment of trochlear palsy. Strabismus. 2004; 12 (2):75-83