Narcotic usage in neonates.
Abstract
Some studies show that each newborn suffers daily from 16 to 35 painful procedures in their hospitalization. Some of these procedures are IV line access, heel stick, intubation, ET tube suctioning, NG lavage, diaper change, repositioning, and minor surgeries such as circumcision. As neonates cannot reflect their pain obviously, we should use attitude and physiologic responses to triggers for pain assessment. These physiologic responses consist of increasing heart rate and blood pressure, intensity of crying, gesture, desaturation, sweating, immune responses, flexion of extremities, change in ICP, increasing catecholamines. Attitude reflections consist of muscle spasms, insomnia, grimaces, change in circadian cycle. The goal of pain relief is to help the newborn adapt to the created circumstance and reduce stress during the procedure. Pain relief can be achieved by pharmaceutical and non-pharmaceutical methods (e.g., surgery) or a combination of these methods based on the specific needs and goals of each patient. Some of the non-pharmaceutical management are sucrose, swaddling, facilitated tucking, Kangaroo Mother Care (KMC), Non Nutritive Sucking, positioning, massage, breastfeeding. Pharmacologic management consists of non-opioid analgesia and opioid analgesia. All of these methods can reduce the pain of newborns and give them a higher quality of life.
Keywords
- neonate
- pain
- non-opioid analgesia
- opioid analgesia
- Kangaroo mother care (KMC)
1. Introduction
The goal of pain relief is to help the neonate adapt to the circumstance and reduce stress during the procedure, so it is important to know and manage the pain procedures. Studies showed that some problems with the best management of pain are due to the unawareness of medical workers of assessment tools and the best way of pain control.
As the researchers want to show and control of any pain in neonates, this review has been collected by the authors. This chapter consists of two parts, pharmaceutical and non-pharmaceutical (massage and breast milk) pain relief, which have been described in detail for readers.
At the end of this chapter, the reader is expected to:
Learn various pain relief methods.
Become familiar with non-pharmaceutical pain relief methods in neonates.
Know the benefits of non-pharmaceutical pain relief methods.
Become encouraged to use non-pharmaceutical pain relief methods in the intensive care unit.
2. Pain management in neonates
Based on the knowledge of recent years, it was thought that neonates have no sense of pain because of myelin deficiency in their nerve fibers and they had many surgeries without any anesthesia, but now a day we know that this defect only causes the retarded transferring of pain signal. Some studies show that each newborn suffers daily from many painful procedures in their hospitalization. As neonates cannot reflect their pain obviously, we should use attitude and physiologic responses to triggers for pain assessment.
Short-term outcomes of pain are change in the circadian cycle, attitude change till 22 hours after a painful procedure, more excitability to following pain, intraventricular hemorrhage, persistent crying, difficulty in falling in asleep, delayed wound healing, changes in immunity, bonding defect, biochemical changes such as hyperglycemia, increasing protein catabolism, increase in cortisol, catecholamine, glucagon, growth hormone, renin, aldosterone, ADH and decrease of insulin.
Long-term outcomes include neurodevelopmental delay, different responses to the same triggers, long-term changes in neurotransmitters, and brain damage. So it is important to know and manage the pain procedures. Studies showed that some problems with the best management of pain are due to the unawareness of medical workers of assessment tools and the best way of pain control.
This chapter will provide these orientations to us.
3. Results and discussion
Pain relief planning for neonates can be accomplished by a multidisciplinary team consisting of doctors, nurses, physiotherapists, and, most importantly, the family. Attention should be paid to the specific role of each member of this team in relieving the newborn’s pain and causing him/her to relax, as well as cooperation and collaboration between the team members and showing enthusiasm in relieving the baby’s pain. Each member of the team may have his/her own unique strategy for detecting and alleviating the baby’s pain, making the coordination between these members and the application of every single method a challenge, which must be discussed before starting the treatment in order to prepare a precise therapeutic plan. Therefore, it is more appropriate to review applicable pain relief methods before starting the treatment and preparing therapeutic plans.
The goal of pain relief is to help the newborn adapt to the created circumstance and reduce stress during the procedure. Pain relief can be achieved by pharmaceutical and non-pharmaceutical methods (e.g., surgery) or a combination of these methods based on the specific needs and goals of each patient. Each of these methods can affect different neuronal pathways involved in pain perception [1].
4. Pharmaceutical pain reduction methods in neonates
The type of pharmaceutical treatment varies depending on the source and severity of the pain, as well as the level of discomfort and side effects of the method.
4.1 Non-opioid analgesia
Aspirin, acetaminophen, ibuprofen, and naproxen can relieve mild to moderate local pain. For neonates that cannot tolerate oral drugs, Ketorolac can be administered intravenously. The dosage is 20–25 mg/kg of body weight for oral acetaminophen and 30 mg/kg when the drug is delivered via the rectal pathway.
4.2 Opioid analgesia
This category of drugs suppresses pain without affecting consciousness and includes opioid analgesics that act on synaptic transporters in different parts of the central nervous system by binding to natural narcotics in the body. These drugs may either block the ascending pain signals in the posterior horn of the spinal cord by affecting the basal ganglia and activating the descending path of pain or cause the pain to become bearable by creating a sensory response to pain through the limbic system.
These drugs include morphine, methadone, pentazocine, propoxyphene, fentanyl, fentanyl citrate, oxycodone, and codeine. The effect of morphine starts only 5 minutes after administration and lasts for up to 15 minutes; however, if this agent is used without a painful stimulus, it may imperil the life of cells (Table 1) [2].
| Name of drugs | Indication | Dosage and routes of administration | Complications | Consideration |
|---|---|---|---|---|
| Fentanyl | Sedation/analgesia, Anesthesia | 0.5–4 mcg/kg Sedation/analgesia per dose IV slow push Infusion rate: 1–5 mcg/kg/h. 5–50 mcg/kg: Anesthesia | Respiratory depression, Chest wall rigidity, Urinary problems | Naloxone should be available |
| Methadone | Opiate withdrawal management | Primary dose: 0.05–0.2 mg/kg every 12–24 h then wean dose 10–20% each week till 4–6 weeks | Respiratory depression, Ileus, Delayed gastric emptying, Long QT interval | Cardiac monitoring, accurate dose decreasing |
| Morphine | Sedation/analgesia, Opiate withdrawal management | 0.05–0.02 mg/kg IV over at least 5 min Start with continuous infusion of 100–150 mcg/kg Till 1 h and then 10–20 mcg/kg/h. Oral dose: 0.03–0.1 mg/kg per dose orally every 3–4 h; wean dose 10–20% every 2/3 days | Respiratory depression, Ileus, Abdominal distention, Urinary problems | Naloxone should be available |
Table 1.
4.3 Local anesthetics
This group of painkillers acts on the cell membrane and disrupts the elevation of the permeability of sodium channels on the axon membrane, a phenomenon that usually occurs after depolarization, preventing the dissemination of the action potential along the axon. Examples of these agents include lidocaine, prilocaine, bupivacaine, chloroprocaine, and tetracaine. Lidocaine and bupivacaine solutions (1– 0.5%) are used in infants at a continuous intravenous infusion dose of 0.2 mg/kg/h. If there is a need for local anesthesia, a dose of 0.5 mL/kg is applicable.
Emla cream contains 2.5% lidocaine and 2.3% prilocaine, and 1–2 g of this cream can be applied for 60–90 minutes prior to vein puncture and painful procedures such as circumcision. Each gram of Emla cream contains 25 mg of lidocaine and 25 mg of prilocaine.
4.4 Regional anesthetics
Anesthetics can sometimes be used as regional blockers, which are applied for nerve blocks via epidural/caudal, dorsal, or intercostal routes. This strategy can be useful in reducing the systemic effects of drugs, particularly when narcotics have led to respiratory complications and apnea. Spinal block is applicable in surgeries below the navel, and epidural/caudal block is used during thoracic, abdominal, and limb surgeries. This type of anesthesia is associated with the risk of incomplete block or neuronal damage, and therefore, it should be performed by appropriately trained anesthesiologists. Today, ultrasound-guided insertion of a needle containing the anesthetic agent offers a novel technique that demands special skills and needs more investigations before it can be recommended for infants.
5. Non-pharmaceutical methods
Studies show the effectiveness of simple non-pharmaceutical methods in relieving pain symptoms. Recently, there has been great emphasis on non-pharmaceutical and non-surgical methods of pain relief as preferable strategies. In premature neonates, non-pharmaceutical methods such as reducing light and noise in the environment and behavioral supports can help mitigate restlessness and reduce the need for painkillers. Furthermore, care training for healthcare staff and parents, including repositioning, sleep regulation, playing music, soft touching, shaking, and non-nutritional sucking, can be effective in reducing stress and the response to pain. Other methods in this area include music therapy, touch therapy, massage, thermal therapy, cryotherapy, aromatherapy, feeding with sucrose and breast milk, etc. In the following, a number of non-pharmaceutical methods frequently suggested for pain control in neonates have been described [3].
5.1 Sucrose
Sucrose is a sweet disaccharide (glucose + fructose) that, by affecting taste receptors located on the tip of the tongue, can trigger the release of intrinsic opioids; however, this agent is not effective when it is administered by injection. Feeding with 2 mL of oral sucrose solution 2 minutes prior to painful procedures has been very helpful in reducing procedural pains. Various studies have shown that oral sucrose has been much more effective than Emla cream, even in premature neonates. Due to the high cost of this agent in our country, it has been recommended that 10% glucose can be a viable alternative with the same efficacy [4].
5.2 Facilitated tucking
In this method, a sheet or a thin blanket is thrown over the baby lying on the bed or inside the nest so that the baby’s organs are completely covered. This method is different from swaddling because it does not restrict the baby’s limb movements.
5.3 Swaddling
This is a very beneficial way to pacify the newborn, especially those older than 31 weeks. In this method, the neonate is completely wrapped in a thin quadrilateral blanket so that only one hand is out of the swaddle. This method is particularly effective in babies who suffer from maternal deprivation syndrome. Also, cuddling babies is facilitated by this method (Figure 1).
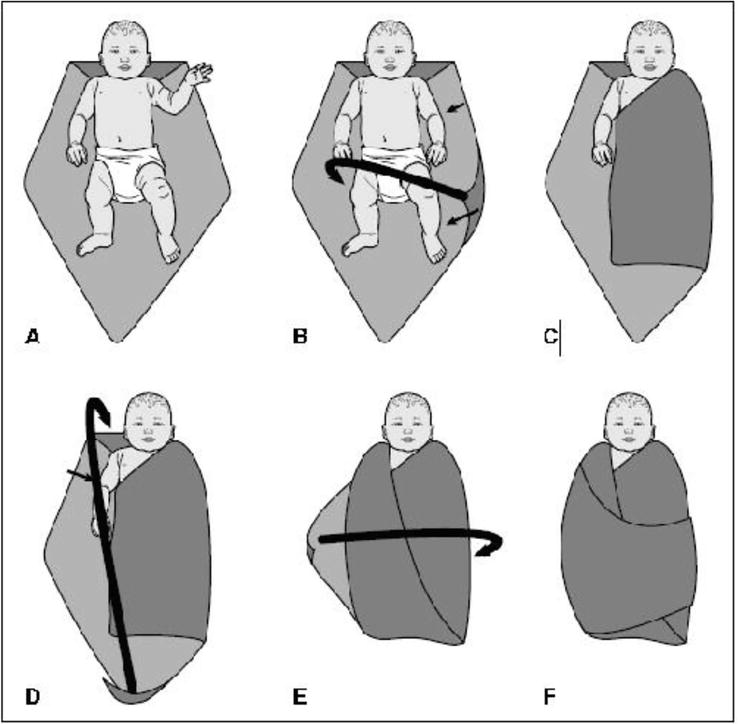
Figure 1.
Method of swaddling. Adopted with permission from clinical handbook of neonatal pain management for nurses, 1st edition, Tara Marko, Michele Dickson, 2016.
5.4 Kangaroo mother care
In 1978 at the Materno Society in Santa, Rey and Martinez presented kangaroo mother care (KMC) as a method recommended for caring for infants. The term KMC is derived from the kangaroo mother care method, where the mother acts as an incubator, and the main nutritional source for the preterm low-birth-weight (LBW) neonates, and the extrauterine life conditions allow the baby to grow similar to term neonates. In KMC, the baby only wears diapers, allowing for direct skin-to-skin contact with the mother, and then a thin bedsheet is laid on them. During KMC, it is better for the mother to sit on a sofa at a 60° angle. This method provides prolonged and continuous touching between the mother and the newborn in the hospital and after discharge and can boost the neonate’s desire for feeding. The KMC method regulates the heart and respiratory rates, deepens sleep, reduces crying and risk of nosocomial infections, improves weight gain and height growth, increases feeding with breast milk, reduces postpartum depression, and also boosts parental satisfaction with the treatment process.
This is also a very effective method in reducing procedural pain in the hospital. In this area, various studies have affirmed the effectiveness of this method in alleviating pain during blood sampling from the heel. In addition, this method can be used in neonates connected to a ventilator or Nasal Continues Positive Airway Pressure (NCPAP).
5.4.1 Objectives of KMC
Boosting newborns’ physical health, especially in premature babies;
Improving the growth and development of the infants hospitalized in the neonatal intensive care unit;
Lowering the levels of stress, depression, and feeling guilty and increasing parents’ self-confidence and abilities while taking care of their premature babies;
Improving the methods of care provision to premature newborns in the hospital and at home;
Nurturing the emotional attachment between the newborn and the parents;
Reducing the duration of hospitalization of the neonate;
Optimizing the use of manpower and technology in the neonatal intensive care unit;
Reducing the rates of nosocomial infections and mortality in hospitals;
Empowering the parents of premature babies to deeply engage them as their babies’ caretakers;
Encouraging feeding with breast milk for premature babies and familiarizing parents with different methods of breastfeeding;
Creating a care team with the participation of parents in order to deliver more effective family-oriented care.
5.4.2 Benefits of KMC
5.4.3 Implementing KMC
5.4.3.1 Skin-to-skin contact
This part includes the direct and long-term (1 hour at first and for longer periods thereafter) contact of the mother’s skin with the baby’s skin, which should be accomplished as soon as possible after birth [5].
5.4.3.2 Physical, emotional, and educational support
The mother, father, and family should be supported by doctors, nurses, midwives, and medical staff. Moreover, receiving support from the community, family, and spouse is particularly needed.
5.4.3.3 Exclusive breastfeeding
This step encompasses supporting and encouraging exclusive feeding with breastmilk, either directly from the mother’s breast or using extracted breastmilk via auxiliary tools such as gastric tubes, syringes, cups, spoons, etc. Most babies weighing below 1500 grams start to gain weight desirably after being exclusively fed with breastmilk.
5.4.3.4 Early discharge and then follow-ups
When KMC care starts in the hospital, it will lead to the early discharge of the premature baby. This type of care can then continue at home. After discharge and in order to ensure the health condition of the baby, parents should refer to the hospital based on a pre-scheduled follow-up plan.
5.4.4 Who can benefit from KMC?
All newborns can receive KMC; however, extremely premature babies requiring special care need to be placed inside a radiant warmer and an incubator, and KMC can be postponed until the neonate’s condition is stabilized.
5.4.5 Noteworthy issues about KMC
Being eligible for receiving KMC depends on several factors. In most cases, birth weight alone can predict who can benefit from this type of care.
Overall, a birth weight of >1200 g is considered suitable for receiving KMC if the following items are met:
An intrauterine age of at least 30 weeks based on LMP and 28 weeks based on the time of fertilization.
The baby’s having a stable hemodynamic condition under mechanical ventilation (if applicable).
The baby’s being kept inside an incubator or a cut.
Babies under the radiant heating device may not be ready for KMC. The use of a warmer device shows that she/he is not yet in a completely stable condition, requiring additional interventions to stabilize the clinical condition.
5.4.6 Step-by-step performing of KMC
Before starting, the mother should consider personal preparations such as emptying the bladder.
The mother’s body temperature should be measured.
Appropriate ambient temperature should be between 21 and 24°C.
The baby’s armpit temperature should be measured, and if it is within the normal and acceptable range, KMC can be initiated.
Necessary tools should be prepared.
A warm and soft four-layer bedsheet should be provided so that if it becomes hot, the thickness can be reduced by removing layers.
A comfortable chair should be provided.
A pulse oximeter should be provided (optional).
Underfoot should be provided.
Small pillows, as needed, should be provided for the mother’s comfort.
Thermometer for check the temperature.
Appropriate clothing for KMC regarding the local culture, the mother’s comfort, and the baby’s safety.
Hat (mandatory for babies weighing less than 1500 g), socks, diapers, and open-front clothes (when the ambient temperature falls below 22°C).
A mirror to see the baby (optional).
5.4.7 Contraindications of KMC
Neonates who are clinically unstable and have fluctuating arterial blood oxygen saturation.
Neonates who have an arterial catheter or chest tube.
Neonates who are predisposed to intraventricular bleeding.
Neonates who receive vasopressor and inotrope drugs.
Neonates bearing a central venous catheter in the shoulder area.
Neonates who suffer from respiratory instability or are under mechanical ventilation.
Babies who have become suddenly ill within 24 hours.
Babies who suffer from persistent apnea and bradycardia require respiratory stimulation.
Parents suffering from cutaneous lesions or ulcers or acute illnesses should postpone this type of care until complete recovery.
Parents who have abnormal physical and mental conditions.
Parents who have not received the necessary training and skills in this field.
5.4.8 The following items should be paid attention to when delivering KMC at home
The ambient temperature should be kept at 21–22°C for term babies and 22–24°C for premature babies.
Although it is easy to perform KMC at home, it requires sufficient skill and knowledge.
The mother can perform her daily work at the same time.
At home, the mother should be encouraged to perform exercise and mental relaxation to achieve peace.
The mother must be familiar with the different methods of breastfeeding a premature baby and acquire the necessary skills at the hospital.
The mother can provide KMC care in a half-seated or half-lying position (on a bed or a chair).
5.5 Cradle rocking
Gently rocking the baby can be very effective in reducing procedural pain. It seems that the mother’s comfortably sitting on a rolling chair while providing KMC can also be very helpful. A study by Amon
5.6 Non-nutritive sucking
Non-nutritive sucking refers to placing a pacifier in the baby’s mouth (i.e., sucking without feeding). According to the valve control theory, the mechanical effect of sucking includes prevention from the transmission of pain impulses to the brain. According to this theory, if either pain is not recognized by the brain or pain signal transmission to the brain is blocked, the negative consequences of pain will disappear. Recent studies conducted on the effect of non-nutritive sucking with sucrose on pain have indicated that the combined use of these methods considerably reduces pain.
5.7 Position
Holding the baby, especially the preterm infant, in its natural position can help reduce pain. Infants tend to be in their fetal position, so they can be supported in such positions with the help of swaddling and tools such as a strap.
5.8 Surroundings
Management of the environment can include reducing the light and noise, avoiding the manipulation of the baby, and managing the sleep-wake cycle, all of which aim to increase relaxation and reduce pain.
5.9 Massage
Throughout history, humans have been using massage to alleviate pain and enhance healing. Massage was first practiced more than 5000 years ago in China and Mesopotamia and is one of the oldest health practices. In 1894, the Association of Trained Massage Therapists was formed, and modern massage therapy techniques were developed worldwide and used for rehabilitation by 1900.
Massage means hitting with the hand and rubbing an organ when a person feels pain or injury. These are almost automatic movements. Cops
Over the years, studies on massage therapy have revealed the pain-reducing effects of this technique, accompanied by increased blood and lymph flow within superficial lymphatic capillaries and improved respiratory function due to the removal of mucus from the respiratory tract.
Massage primarily facilitates blood flow. When muscles are rubbed and subjected to tension, they expedite blood return to the heart, driving acids such as lactic acid out of the muscle tissue. In addition, improved blood flow enhances tissue perfusion and oxygenation. Massage also induces the release of endorphins (i.e., natural analgesics) in the body.
5.9.1 Evidence on the effects of massage therapy
Recently, a systematic review on the role of tactile stimulation in healthy infants revealed that massage during infancy might have beneficial effects on sleep and crying patterns, neonatal stress levels, circadian rhythms, mother-infant interaction, and neonatal development and well-being.
5.9.2 Massage and procedural pain
Infants are likely to experience one of the numerous painful procedures while receiving routine health care, such as heel blood sampling heel, circumcisions, and vaccination. These painful procedures during infancy and childhood may influence the child’s response to pain in the future. In studies on the infants undergoing heel blood sampling, fewer facial expressions and a lower increase in the heart rate were observed in the infants receiving massage compared to their peers in the control group [6].
5.9.3 Massage in low-birth-weight infants
Various studies (n = 14) have reported that massage can reduce hospital stays and improve weight gain. In LBW neonates, massage can improve sleep quality, reduce stress behaviors, enhance vagal activity and gastrointestinal tract movements, and increase the levels of insulin and insulin-like growth factors.
There is ample evidence supporting the beneficial effects of massage therapy on anxiety, depression, complications of autism spectrum disorders, chemotherapy side effects, diabetes symptoms, rheumatoid arthritis pain, and pulmonary function in adults and, to a lesser extent, in children; however, there are no such studies on neonates.
Five basic techniques are used in massage therapy, including:
Floorage
Petrissage
Friction
Tapotement
Vibration
Ling and Mezger defined floorage as stroking, which is a movement during which the hand slides over the skin without moving the deep muscles. Also, petrissage is a rubbing and pressing movement where the muscles are grasped and raised by the hand. This movement mitigates muscle pain by discarding lactic acid and boosting muscular blood flow. During friction, the masseur uses the thumbs and other fingertips to work around the joints, as well as the thickest parts of the muscles.
In the tapotement technique, the masseur uses the margins of the hands, fingers, and palms (formed as cup-like) to introduce tiny, professional, and strip movements. Generally, tapotement refers to any rapid and consecutive tapping aiming to stimulate the local blood flow and induce hyperemia, as well as prolonged tapping leading to muscle exhaustion and relaxation.
During vibration, the therapist’s open hands are firmly placed on the muscle, leading to rapid local vibrations for several seconds. This movement continues until the entire muscle vibrates and helps stimulate the nervous system, boosting blood flow and improving endocrine function.
5.9.4 Mechanism of action of massage therapy
The mechanism of action of massage therapy has not been fully understood in children, infants, or adults. One hypothesis suggests that massage therapy may promote biochemical changes in soft tissues, including elevated blood flow and oxygenation of muscles and connective tissues. Recent studies have proposed that massage can increase the level of oxytocin hormone and nurture a feeling of well-being, leading to a reduction in anxiety. The pain-relieving effects of massage therapy may also be due to the secretion of endorphins and serotonin. Another hypothesis states that massage can stimulate thick neuronal fibers, suppressing the thin neuronal fibers interacting with pain receptors, which exactly mimics the valve control mechanism [7].
5.9.5 Benefits of massage therapy
Alleviating procedural pains;
Reducing anxiety and depression;
Reducing stress;
Improving weight gain in premature neonates;
Reducing the risk of autism in premature neonates;
Improving pulmonary function;
Relaxation and stabilization of vital signs;
Reducing cardiac dysrhythmias;
Accelerating the healing of bone fractures;
Improving tension headaches;
Treatment of anemia;
Acceleration of wound healing;
Reducing joint pain and improving joint function in neonates suffering from degenerative arthritis and osteoarthritis.
5.10 Breastfeeding and breast milk
Aside from the methods already mentioned, breastfeeding is one of the physiological methods of pain reduction in infants. The benefits of breastfeeding are numerous. Breastfeeding has significantly reduced morbidity and mortality during infancy and childhood worldwide and has contributed to the health of communities beyond perceptions and expectations. Studies have shown that infants breastfed enjoy numerous short-term and long-term benefits due to the presence of a variety of essential biomolecules in breast milk. On the other hand, infants who remain deprived of milk or breast milk generally require costly treatments in the hospital.
The infant benefits not only from the breast milk itself but also from the mechanical action of breastfeeding. The infant should completely open his/her mouth and place the tongue in the lower part of the lower gum in order to breastfeed effectively. While the tongue remains in this position, a wave-like movement starts along the length of the tongue (from the tip to the bottom). The breast tissue is placed inside the infant’s mouth, and due to the pressure caused by the wave-like movement against the breast tissues facing the hard palate, milk starts to pour out from its reserves (lactiferous sinuses) into the infant’s throat, where the act of swallowing takes place. So, it seems that the sucking actions taking place to squeeze out milk from the mother’s breasts can optimally exercise the soft palate muscles.
Some of these factors inevitably interfere with effective oral feeding; nevertheless, breastfeeding is easier to establish and succeed than bottle feeding. Coordination between reflexes, sucking, swallowing, and breathing may be influenced by severe prematurity or underlying diseases.
Multiple studies have declared that breastfeeding affects the response to pain in a sensory-oral way. Also, it has been reported that breastfeeding is one of the natural ways to reduce pain depending on skin-to-skin contact, sucking, and the sweetness of the milk. Recent studies have noted that special and pleasant flavors can reduce pain in neonates. Breast milk (less than 2 mL), along with its proteins, fats, and sweeteners, can effectively lower pain and spontaneous crying in human and mouse infants.
5.10.1 The role of nurses in reducing pain in neonates
It is critical for nurses to intervene in treating pain and preventing its short- and long-term complications in neonates exposed to severe and recurring pain. Regarding professional ethics, nurses are responsible for recognizing and alleviating pain in newborns who are inevitably exposed to pain or in those who are under intubation and unable to express pain by crying. Compared to others, nurses are closer to hospitalized patients, placing them in the best position for detecting, preventing, and treating pain.
5.10.2 Action mechanisms of non-pharmaceutical analgesics
Several mechanisms are presumed for the analgesic effects of non-pharmaceutical pain-relieving interventions. One hypothesis that probably is true for all of these methods considers the valve control theory proposed by Malzak and Wall, according to which stimuli that pass through the ascending routes can suppress pain signal receptors following painful stimuli by employing various intrinsic pathways related to the thalamus of the spinal cord. The stronger these competitive stimuli are, including in the case of multifaceted methods, the more effective they can be in pain perception inhibition. This theory explains why multifaceted interventions, such as kangaroo care, breastfeeding, or sensory saturation (involving tactile, auditory, and olfactory mechanisms) are more effective than individual stimuli (e.g., auditory or olfactory alone). Another mechanism for pain reduction engages the upper parts of the brain and is related to the release of endorphins. Endorphins are released following stress (including pain) or positive stimuli such as touching. For instance, sucrose, due to its sweetness, is believed to induce the release of endorphins. On the other hand, sucking seems to involve mechanical routes (according to valve control theory) in order to prevent the transmission of pain impulses to the brain. According to this theory, the negative consequence of pain wanes if the pain is not perceived by the brain or the transmission of pain signals to the brain is blocked. For various painful procedures, the respective pain-relieving measures can be categorized as noted so that the newborn can benefit from an appropriate palliative treatment (Table 2).
| Management | Analgesia-anesthesia | Opiate analgesia | Oral sucrose | Emla cream | Non-pharmacologic pain relief |
|---|---|---|---|---|---|
| Heal stick | × | × | |||
| Venipuncture | × | × | × | ||
| Intramuscular or Subcutaneous injection | × | × | |||
| IV cannulation | × | × | × | × | |
| Arterial puncture & peripheral arterial line | × | × | × | ||
| Umbilical catheterization | × | × | |||
| Lumbar puncture, Arterial or Venus cut down | × | × | × | ||
| Peripherally inserted central catheter | × | × | × | × | × |
Table 2.
Classification of pain control in any painful procedure in neonatal ward.
5.10.3 Necessary recommendations for better pain management in neonatal intensive care units
A written clinical guide should be present in every neonatal intensive care unit (NICU), and specific palliative measures should be presented for every painful procedure.
Non-pharmaceutical pain-reducing methods, such as kangaroo care, swaddling, nesting, oral sucrose, and massage, should be performed in NICUs.
One should try to eliminate stressful stimuli (auditory, vision, touch, and balance), especially light and excessive noise, in NICUs.
If applicable, blood sampling should be from the heel.
In order to reduce pain during catheterization, the specific clinical guide of the same catheter should be used.
All healthcare workers are required to pass courses on neonatal pain reduction and be aware of the dire consequences of failing to relieve procedural pain.
6. Conclusion
At the end of this chapter, authors hope that they can present a qualified program to pain management of newborns and give them a higher quality of life.
References
- 1.
Shepherd TB, Tobias JD. Neonatal pain management. Saudi Arabia Journal of Anaesthesia. 2014; 8 (Suppl 1):S89-S97 - 2.
Attarian S, Tran LC, Moore A, Stanton G, Meyer E, Moore RP. The neurodevelopmental impact of neonatal morphine administration. Brain Sciences. 2014; 4 :321-334 - 3.
Riddell RP. Nonpharmacological management of procedural pain in infants and young children: An abridged Cochrane review. Pain Research & Management. 2011; 16 (5):321-330 - 4.
Effe E, Ozer ZC. Effect of sucrose on pain relief during neonatal immunization injection. Applied Nursing Research. 2007; 20 (1):10-16 - 5.
Gray L, Watt L, Blass EM. Skin-to-skin contact is analgesic in healthy newborns. Pediatrics. 2000; 105 :e14 - 6.
Zargham-Boroujeni A, Elsagh A, Mohammadizadeh M. The effects of massage and breastfeeding on response to venipuncture pain among hospitalized neonates. Iranian Journal of Nursing and Midwifery Research 2017; 22 (4):308-312 - 7.
Tiffany Field. Touch for socioemotional and physical well-being: A review. Developmental Review. 2010; 30 :367-383