Distribution of time of injury.
Abstract
Background: Determining injuries in relation to death have been highly imperative to forensic anthropologist since they provide clues on the norms, cultures and pattern of death of an individual. Aim: The study aimed at determining injuries among skeletal elements in the Anatomy Musuem of Delta State University, Abraka, Nigeria. Methodology: The study was crosssectional and a total of 150 bones which included the skulls, calvarium and pelvis were examined for the presence of ante, peri and postmortem injuries. Other injuries such as blunt force, sharp force and ballistic injuries were also studied. Chisquare test was used to evaluate an association between the bones and the time of injuries. Statistical assessment was done using SPSS 21 Software Version. Significance was accepted at p < 0.05. Result: The study showed that postmortem injuries was the most predominant (98%) among the bones. This was followed by perimortem and antemortem injuries (11.3, 10%). The percentages of blunt force, ballistic and sharp force were 98, 1.3 and 0.7% respectively. Further findings showed that there was no association between the bones and the nature of injuries that were observed (p = 0.837; 0.713). Conclusion: The study had shown that there are so many hidden facts from skeletal remains which can be of vital importance to forensic science.
Keywords
- antermortem
- perimortem
- postmortem
- injuries
- Delta State
- Nigeria
1. Introduction
Investigating bones for injuries have become a vital tool in forensic studies [1]. They can establish an individual’s identity when compared with past medical records or ascertain the circumstances of death [1]. These injuries can be classified into ante-, peri- and postmortem depending on the time of occurrence [2, 3, 4]. Injuries are termed antemortem when they occur before death and are evidenced with partial or complete healing, visible at the fracture edges of bones as compared to peri-mortem injuries that show no signs of healing [1, 3, 5, 6]. Peri-mortem injuries occur at the time of death and they are distinguished in bones by the presence of fractures that interpret the cause death [1]. According to Elena [1], they are expressed by plastic deformation seen at the site of injury. Peri-mortem injuries also present a soft preponderant texture and regular outline as compared to postmortem injuries that are characterized with a rough preponderant texture and outline [1, 7, 8, 9]. It has been documented that postmortem bones have fracture patterns that are squared with sharp edges that are likely to cause enormous disintegration on dry bones [1, 7, 8, 9]. Post damages on bones classically reveal right-angled fractured margins, while those of peri-damages show obtuse or acute fracture angles [1, 7, 8, 9]. This have also been confirmed from computed tomographic scans [10]. It has also been acknowledged that injuries can also be blunt force, sharp force, ballistic and thermal [4]. This depends on the instruments that cause death at different time frame [1]. The blunt force injuries have been described as the most frequent type of injuries and they are associated with blunt objects or surfaces [1]. It must be frazzled that forensic assessment of dead bodies for injuries have now become a regular task for forensic pathologists, medical examiners and forensic anthropologists in various countries. Currently, examination of injuries includes the evaluation of ante-, peri-, or postmortem injuries, identification of injury patterns as well as possible association with certain objects. They have been limiting information on assessing injuries from remains of corpses in Nigeria, hence this study investigated them on dry bones in the Anatomy Museum of Delta State University, Abraka, Delta State Nigeria.
2. Materials and methods
The study was crosssectional and a total of 150 bones which included the skulls, calvarium and pelvis were investigated for the presence of ante-, peri- and postmortem injuries. They were also examined for other injuries such as the blunt force, sharp force and ballistic injuries. Data were represented in frequencies and percentages while a Chisquare test showed an association between bones and the time of injuries. Ethical approval for this work was obtained from the Department of Human Anatomy, Faculty of Basic Medical Sciences, Delta State University, Abraka, Delta State.
3. Results and discussions
Table 1 showed that 78.7, 11 and 10% of the bones had post-, peri- and antemortem injuries. Findings also showed that blunt force (98%), ballistic injuries (13%) and sharp force damages were observed among the investigated bones (Table 2). Table 3 presented 45.3% calvariums, 10% pelvis, 44.7% skulls while Table 4 illustrated the injuries that were present among these bones. It can be depicted fromTable 4 that 8.8, 20, 9%; 10.3, 13.3, 11.9%; 80, 66.7, 79.1% of the calvarium, pelvis and skull bones had ante-, peri- and postmortem injuries. Other injuries that were observed were blunt force, ballistic and sharp force (Table 5). These injuries were specific to the bones that were studied. According to Table 5, ballistic injuries was explicit on the skull and calvaria bones (98.5, 1.5%) while sharp force was specific to the calvarium (1.5%). Blunt force injury was noted on the calvarium (97%), pelvis and skull (100%) each respectively. Further findings showed that there was no association between injuries and the skeletal elements invested (p = 0.837; 0.713
| Time of injury | Frequency (%) |
|---|---|
| Antemortem | 15 (10.0) |
| Perimortem | 17 (11.3) |
| Postmortem | 118 (78.7) |
| Total | 150 (100.0) |
Table 1.
| Nature of injury | Frequency (%) |
|---|---|
| Sharp force | 1 (0.7) |
| Blunt force | 147 (98.0) |
| Ballistic force | 2 (1.3) |
| Total | 150 (100.0) |
Table 2.
Distribution of nature of injury.
| Skeletal elements | Frequency (%) |
|---|---|
| Calvarium | 68 (45.3) |
| Pelvis | 15 (10.0) |
| Skull | 67 (44.7) |
| Total | 150 (100.0) |
Table 3.
Distribution of examined skeletal elements.
| Skeletal elements | Frequency | (%) | |
|---|---|---|---|
| Calvarium | Antermorterm | 6 | 8.8 |
| Perimorterm | 7 | 10.3 | |
| Postmorterm | 55 | 80.9 | |
| Total | 68 | 100.0 | |
| Pelvis | Antermorterm | 3 | 20.0 |
| Perimorterm | 2 | 13.3 | |
| Postmorterm | 10 | 66.7 | |
| Total | 15 | 100.0 | |
| Skull | Antermorterm | 6 | 9.0 |
| Perimorterm | 8 | 11.9 | |
| Postmorterm | 53 | 79.1 | |
| Total | 67 | 100.0 | |
| ( | |||
Table 4.
Distribution of examined skeletal elements based on time of injury.
| Skeletal elements | Frequency | (%) | |
|---|---|---|---|
| Calvarium | Ballistic force | 1 | 1.5 |
| Blunt force | 66 | 97.1 | |
| Sharp force | 1 | 1.5 | |
| Total | 68 | 100.0 | |
| Pelvis | Blunt force | 15 | 100.0 |
| Total | 1 | 1.5 | |
| Skull | Ballistic force | 66 | 98.5 |
| Blunt force | 67 | 100.0 | |
| Total | 1 | 1.5 | |
| ( |
Table 5.
Distribution of examined skeletal elements based on nature of injuries.
| Skeletal elements | Nature of injury | Chi-square | Df | P-value | ||
|---|---|---|---|---|---|---|
| Ballistic force | Blunt force | Sharp force | ||||
| Calvarium | 1 (0.7) | 66 (44.0) | 1 (0.7) | 1.442 | 4 | 0.837 |
| Pelvis | — | 15 (10.0) | — | |||
| Skull | 1 (0.7) | 66 (42.0) | — | |||
Table 6.
Chi-square test of association between time of injury and nature of injury.
| Skeletal elements | Time of injury | Chi-square | Df | P-value | ||
|---|---|---|---|---|---|---|
| Antemortem | Perimortem | Postmortem | ||||
| Calvarium | 6 (4.0) | 7 (4.7) | 55 (36.7) | |||
| Pelvis | 3 (2.0) | 2 (1.3) | 10 (6.7) | 2.125 | 4 | 0.713 |
| Skull | 6 (4.0) | 8 (5.3) | 53 (35.3) | |||
Table 7.
Chi-square test of association between injury time and examined skeletal elements.
The study had shown that all bones that were studied had more postmortem damages. Features that were observed for this injury were desiccation and fragility. This could be as a result of exposure of these bones to the environment. Several authors are of the opinion that changes that occur to corpses after death are due to complex results from physicochemical and environmental processes [1, 4]. They are affected by factors surrounded by the cadaver and the environment that they are kept [1, 4]. These factors influence the onset, increases the pace of post-mortem changes or impede it. The bones we observed having blunt force had an impact region, cranial and facial fractures. These evidences were highlighted by Casali
4. Conclusion
It has been established that several injuries discovered on bones can be of immense value to forensic anthropologist in investigating crimes, nature of death of an individual as well as tell a people way of life because of the instruments associated with the death of an individual (Figures 1 and 2).
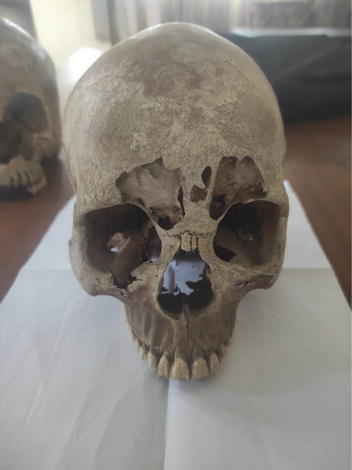
Figure 1.
A skull illustrating blunt force injury.

Figure 2.
A calvarium illustrating sharp force injury.
References
- 1.
Elena FK. Forensic investigation of cranial injuries due to blunt force trauma: Current best practice. Journal of Research and Reports in Forensic Medical Science. 2015; 5 :25-37 - 2.
Sauer N. The timing of injuries and mannerof death: Distinguishing among antemortem, perimortem, and post-mortem trauma. In: Reichs KJ, editor. Forensic Osteology: Advances in the Identification of Human Remains. 2nd ed. Springfield, IL: Charles C. Thomas; 1998. pp. 321-332 - 3.
Rodriguez-Martin C. Identification and differential diagnosis of traumatic lesions of the skeleton. In: Schmitt A, Cunha E, Pinheiro J, editors. Forensic Anthropology and Medicine: Complementary Sciences from Recovery to Cause of Death. New Jersey: Humana Press; 2006. pp. 197-221 - 4.
Galloway A. The biomechanics of fracture production. In: Galloway A, editor. Broken Bones: An Anthropological Analysis of Blunt Force Trauma. Springfield, IL: Charles C. Thomas; 1999. pp. 35-62 - 5.
Iscan MY, Steyn M, editors. The Human Skeleton in Forensic Medicine. 3rd ed. Springfield, IL: Charles C. Thomas; 2013 - 6.
Lovell NC. Trauma analysis in paleopathology. Yearbook Physical Anthropology. 1997; 40 :139-170 - 7.
Dirkmaat DC, Cabo LL, Ousley SD, Symes SA. New perspectives in forensic anthropology. Yearbook Physical Anthropology. 2008; 51 :33-52 - 8.
Morlan RE. Toward the definition of criteria for the recognition of artificial bone alterations. Quaternary Research. 1984; 22 :160-171 - 9.
Fleming-Farrell D, Michailidis K, Karantanas A, Roberts N, Kranioti EF. Virtual assessment of perimortem and postmortem blunt force cranial trauma. Forensic Science International. 2013; 229 (1-3):162.e1-162.e6 - 10.
Bonnichsen R. Pleistocene Bone Technology in the Beringian Refugium. National Museum of Man Mercury Series, Archaeological Survey of Canada Paper No 89. Ottawa, Canada; 1979 - 11.
Casali MB, Battistini A, Blandino A, Cattaneo C. The injury pattern in fatal suicidal falls from a height: An examination of 307 cases. Forensic Science International. 2014; 244 :57 - 12.
Byers SN. Introduction to Forensic Anthropology: A Textbook. 2nd ed. Pearson Education: Boston, MA; 2005 - 13.
Aufderheide AC, Rodriguez-Martin C. The Cambridge Encyclopedia of Human Paleopathology. Cambridge: Cambridge University Press; 1998 - 14.
Konstantinos M, Chara S. Identification and differentiation diagnosis of perimortem blunt force trauma in tubular long bones. Forensic Science Medical Pathology. 2006; 2 (4):221-230 - 15.
Smith OC, Pope EJ, Symes SA. Look until you see: Identification of trauma in skeletal material. In: Steadman DW, editor. Hard Evidence: Case Studies in Forensic Anthropology. Upper Saddle River, NJ: Prentice Hall; 2003. pp. 138-154 - 16.
Berryman HE, Symes SA. Recognizing gunshot and blunt cranial trauma through fracture interpretation. In: Reichs KJ, editor. Forensic Osteology: Advances in the Identification of Human Remains. Springfield, IL: Charles C. Thomas; 1998. pp. 333-352 - 17.
Thompson TJU, Inglis J. Differentiation of serrated and non-serrated blades from stab marks in bone. International Journal of Legal Medicine. 2009; 123 (2):129-135