Characteristics of 142 ARMs patients and post-operative functional outcomes.
Abstract
Three-dimensional high-definition manometry was used in evaluating anorectal function of 142 post-operative patients with anorectal malformations (ARMs), while 104 non-operative children as controls (CON) who were subdivided into different age groups. Data were collected on the functional length (HPZ-length), resting and squeeze pressure (HPZ-rest, HPZ-sqze), recto-anal inhibitory reflex (RAIR), and strength distribution of the anal canal. The results showed a gradual increase in anal canal function parameters with age in normal infants and children, suggesting that age should be considered as an essential factor when evaluating post-operative anorectal function in ARMs patients. Comparing with CON, a significant decrease in HPZ-rest was observed in all post-operative ARMs groups (p < 0.05). The majority of ARMs patients with incontinence had significantly lower HPZ-rest and a higher percentage of asymmetric strength distribution compared to those with continence (p < 0.05). The type classification of high and cloaca in ARMs, as well as low HPZ-rest, were identified as two factors affecting post-operative functional outcomes. Manometry is a valuable modality providing distinct details of anal function in the assessment of the underlying functional causes of postoperative defecation disorder, thus helping physicians select the right modality of treatment. Sequential manometry studies are useful for re-evaluating anal function after treatment and biofeedback training.
Keywords
- anorectal manometry
- anorectal function
- anorectal malformation
- post-operative anal function
- long-term post-operative complication
1. Introduction
Congenital anorectal malformations (ARMs) are developmental malformations of the end digestive tract, with an incidence of 3.17 cases per 10,000 population in China, and 1 case per 5000 live births worldwide [1, 2]. Subsequent surgical interventions in early infancy can be mild, severe, or complex, depending on the type of classification of ARMs. Their post-operative functional outcomes varied, even though they had been treated excellently by the surgery. In other words, ARMs are anatomical or structural abnormalities that need to be repaired, but they are not abnormalities that can simply be corrected by definitive surgery. Whether the reconstructed anus will gain bowel function similar to that of the average person is the most critical concern of both parents and surgeons. Once post-operative complications occur, especially in those with minor abnormalities, parents may be suspicious of surgical management, while surgeons may blame poor development of the anorectum itself.
Constipation and fecal incontinence are common functional complications seen during long-term follow-up. Normally, the post-operative function is assessed using the conventional clinical scoring system based on subjective parameters, such as the number of defecation and the ability to have voluntary bowel movement [3, 4]. Poor scores undoubtedly reflect impaired anorectal function, but they are not a reliable criterion for assessing the outcome of surgical treatment or the function of the reconstructed anorectal canal. In the latter case, a variety of factors are involved in bowel movement, such as the development of muscle complexes, rectal sensation, and reflexes. Even an improper diet may cause constipation or soiling.
Image studies such as ultrasound, MRI, contrast enemas, and manometry are the objective assessment methods commonly used to evaluate the function of the newly constructed anorectal canal. Ultrasound and MRI are studies concerning the anatomical structure (e.g. the position of the constructed anorectal canal) and the development of the muscle complex, whereas the enema and manometry provide valuable information about bowel movement. Recently, three-dimensional (3D) high-definition anorectal manometry has been believed to be a precise tool for assessing defecation function because it provides quantitative objective measurements in real-time and dynamically [5, 6]. It offers imaging and helps understand the functional and potential pathophysiology of functional anorectal disorders. In this chapter, we present our study of the use of 3D high-definition manometry in the evaluation of anal canal function in ARMs patients and their non-operative controls.
2. Materials and methods
2.1 Patients
2.1.1 Non-operative control
Non-operative control (CON) patients enrolled were those who underwent 3D manometry at Beijing Children’s Hospital from November 2014 to January 2019. Inclusion criteria are as follows: patients without organic anorectal diseases (as determined by imaging studies and rectal mucosal biopsy) are included; and patients have normal bowel habits during clinical follow-up though they had manometry exams because of irregular bowel movements. Exclusion criteria included patients with Hirchsprung’s disease (HD) and those with a history of anorectal-related surgery, with spinal cord or vertebral deformity. Of these controls, 71 children were selected as the age-matched CON when compared to patients with post-operative ARMs.
2.1.2 Congenital anorectal malformations patient
We conducted a retrospective review of all patients with ARMs admitted to Beijing Children’s Hospital between January 2015 and December 2019. A total of 171 measurements were performed on 142 post-operative patients who received follow-up at our outpatient clinic. Among them, 10 patients who had previously undergone surgical repair at their local hospitals came to our clinic because of poor post-operative outcomes. The remaining 132 patients who underwent surgery at our hospital were subjected to routine follow-up starting 3 months after surgery, regardless of the presence of complications. Repeated manometric examinations were conducted on patients with impaired bowel function, either after conservative management or simply as they advanced in age.
Post-operative outcomes were rated as good, fair, or poor based on a patient’s bowel movements. “Good” refers to the condition in which patients have regular bowel movements without any complaint of defecation. “Fair” refers to mild and controllable constipation and soiling conditions. In the former, constipation is treatable with oral medication or laxatives, while in the latter, only occasional episodes of dirty pants may occur during sleep, coughing, or diarrhea. “Poor” indicates severe constipation and frequent incontinence to the extent that regular bowel management is often needed.
2.1.3 Classification of patients
General information on the types of ARMs and their surgical management was obtained through an electronic medical record system. At the outpatient follow-up clinic, manometry measurement was conducted following a physical examination. Both CON and ARMs patients were asked to complete a questionnaire about their dietary and bowel habits. In manometric examination, non-operative CON were divided into four groups based on age: ≤1 month, 1–12 months, 1–4 years, and > 4 years. The rules of age grouping were quoted from our previous study [7] and those of others. The age divisions of less than 1 month and 1 month to a year were selected in accordance with Kumar’s study [8], while the next dividing age four was originated from the Rome IV questionnaire [9]. The studies were approved by the Medical Ethics Committee of Beijing Children’s Hospital (2018-K-129), and the patient consent requirement was waived.
2.2 Anorectal manometry
A high-definition manometry catheter (ManoScan 360HD, Sierra Scientific Instruments, Los Angeles, California) was used to determine the mean pressure of the anal canal with the implemented Smartmouse™ and its software algorithm (ManoView analysis software, Sierra Scientific Instruments, Los Angeles, California). The patient lays either supine or in a lateral position. A lubricated catheter (10.75 mm in diameter, 6.4 cm in length equipped with 256 pressure sensors in 16 rows and 16 circumferentially oriented) was inserted into the anus and the pressure was calibrated to the baseline position. When the proximal and distal ends of the high-pressure zone were established with the aid of the Smartmouse™, the following parameters were collected: (1) the length of the anorectal high-pressure zone (HPZ-length); (2) the mean resting pressure (HPZ-rest); (3) the mean squeeze pressure (HPZ-sqze), via measuring passive contractions induced by applying perianal pricks in patients under 4 years of age and voluntary contraction in those older than 4; (4) recto-anal inhibitory reflex (RAIR), RAIR was considered positive when a decrease of 25% or more in the resting pressure was achieved; (5) the strength distribution of the anal canal, as shown in Video 1 (https://bit.ly/3IkMJxs), in which the anal pressure and strength distribution could be viewed and calculated in the 2D topographic color plot of all pressure transducers when the 3D column plot was cut along the anterior line. Detailed anorectal manometry procedures can be quoted from our previous study [7]. All procedures were performed by the same registered nurse, and the results were analyzed by two senior physicians.
2.3 Statistical methods
All analyses were performed using SPSS, version 23.0 (IBM Corp, Armonk, NY), in which statistical significance was considered when the
3. Results
3.1 Congenital anorectal malformations patients (ARMs)
One hundred forty-two patients (61 boys and 81 girls) ranging in age from 3 months to 15 years (median 1.71 years) were included in the surgery group. Based on the level of the rectum in relation to the levator ani muscle, the ARMs were classified into high (10%), intermediate (28%), and low type (62%) by Wingspread classification [10, 11]. Types of fistulas were classified as follows: no fistula (1%); anocutaneous fistula (42%); rectovestibular fistula (25%); rectobulbar-urethral fistula (17%); rectoprostatic-urethral fistula and rectovesical fistula (5%); rectovaginal fistula (6%); and cloaca (4%). Post-operative fecal continence was socially acceptable in 80% of the patients, 50% of whom having good functional outcomes, and 30% having fair ones. The remaining 20% were patients with poor outcomes, in which fecal incontinence and severe constipation were seen, with the former cases more than the latter. The detailed patient information presented in Table 1 is derived from our previous study [12].
| Good (n = 72) | Fair (n = 42) | Poor (n = 28) | ||||
|---|---|---|---|---|---|---|
| Constipation (n = 20) | Soiling (n = 22) | Severe constipation (n = 8) | Incontinence (n = 20) | |||
| Male:female | 32:44 | 7:13 | 10:12 | 3:5 | 9:11 | |
| Low | Without fistula | 1 | 0 | 0 | 0 | 1 |
| Anocutaneous fistula | 34 | 11 | 10 | 2 | 3 | |
| Anovestibular fistula | 17 | 3 | 3 | 2 | 1 | |
| Intermediate | Without fistula | 0 | 0 | 0 | 0 | 0 |
| Rectobulbar-urethral fistula | 12 | 1 | 5 | 1 | 5 | |
| Rectovestibular fistula | 2 | 1 | 1 | 3 | 3 | |
| Rectovaginal fistula | 3 | 2 | 0 | 0 | 1 | |
| High | Without fistula | 0 | 0 | 0 | 0 | 0 |
| Rectoprostatic-urethral fistula/rectovesical fistula | 2 | 0 | 2 | 0 | 3 | |
| Rectovaginal fistula | 0 | 0 | 1 | 0 | 1 | |
| Cloaca | 1 | 2 | 0 | 0 | 2 | |
| Associated spinal/vertebral deformity | 10 | 6 | 4 | 5 | 6 | |
Table 1.
“Good” refers to regular bowel movement. “Fair” refers to constipation but could be solved by oral medication or laxatives, as well as occasional dirty pants occurred during sleep, cough, and diarrhea. “Poor” refers to severe constipation that bowel management (e.g., enema) was needed, whereas incontinence refers to a recurrent involuntary loss of liquid and/or solid stool in older children and frequent dirty pants in toddlers.
3.2 Anorectal manometry of the anorectal canal
3.2.1 General information of manometry in ARMs patients vs. CON
Quoted from our previous studies, the results of the correlation analysis between age and manometric parameters in non-operative CON revealed a positive correlation between age and manometric parameters, specifically HPZ-length, HPZ-rest, and HPZ-sqze measurements, indicating that anal length and pressure were influenced by advancing age (Figure 1). When the reconstructed anal canal were compared with their age-matched non-operative CON, significantly lower HPZ-rest was observed in all post-operative groups (Table 2) [12].
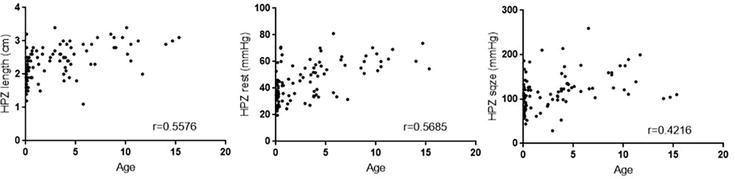
Figure 1.
Scatter plot with linear trend line for age and HPZ-length, HPZ-rest, and HPZ-sqze in CON.
| Age group | Number | HPZ-length (cm) | P-value | HPZ-rest (mmHg) | P-value | HPZ-sqze (mmHg) | P-value | |||
|---|---|---|---|---|---|---|---|---|---|---|
| ARMs:CON | ARMs | CON | ARMs | CON | ARMs | CON | ||||
| 3–12 m | 30:16 | 2.48 ± 0.46 | 2.32 ± 0.34 | 0.172 | 32.72 ± 12.30 | 43.94 ± 14.86 | 0.002* | 108.11 ± 35.35 | 114.59 ± 34.60 | 0.525 |
| 1–4y | 82:24 | 2.65 ± 0.52 | 2.45 ± 0.42 | 0.099 | 28.08 ± 10.54 | 43.05 ± 11.12 | <0.001* | 99.78 ± 35.13 | 107.90 ± 45.30 | 0.410 |
| >4y | 30:31 | 2.69 ± 0.60 | 2.64 ± 0.50 | 0.713 | 28.38 ± 11.90 | 55.97 ± 12.72 | <0.001* | 91.04 ± 29.74 | 141.46 ± 35.69 | <0.001* |
| Total | 142:71 | 2.57 ± 0.51 | 2.50 ± 0.45 | 0.307 | 30.43 ± 11.80 | 48.89 ± 14.03 | <0.001* | 102.61 ± 34.84 | 125.09 ± 41.21 | <0.001* |
Table 2.
Comparison of basic manometric parameters between ARMs patients and non-operative CON.
The difference was statistically significant.
HPZ-length: the functional length of anorectal high-pressure zone; HPZ-rest: resting pressure of high-pressure zone; HPZ-sqze: squeeze pressure of high-pressure zone. Data was reported as mean ± standard deviation.
In the study of anal strength distribution, asymmetric pressure distribution could be observed in both resting and contracting periods in patients, and even in the CON. Meanwhile, asymmetric strength distribution was also frequently seen in ARMs group regardless of surgical approaches taken (Video 2, https://bit.ly/3IkMJxs). When compared to CON, a significantly higher percentage of the asymmetric strength distribution was seen in ARMs patients during both resting and squeezed phases (Video 3, https://bit.ly/3IkMJxs).
3.2.2 Comparison between good and poor functional outcomes in ARMs patients
Figure 2 shows our previous statistic results indicating that the incontinence ARMs individuals had significantly higher proportions of lower HPZ-rest, negative RAIR, and asymmetric distribution in the squeeze phase [12]. As there were no significant differences observed in the manometric parameters among adjacent age groups in ARMs patients, the mean values of each measurement were calculated and compared between the “Good + Fair” and “Poor” function groups, as well as CON. As shown in Table 3, all parameters of the functional “Good + Fair” group were comparable with CON, while significantly lower HPZ-rest and HPZ-sqze were observed in the functional “Poor” group.
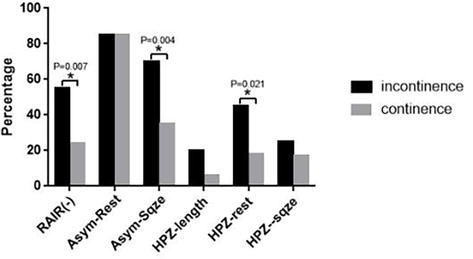
Figure 2.
Statistic results of comparing the patient number of the poor manometric parameter in ARMs between incontinence and continence group.
| HPZ-length (cm) | HPZ-rest (mmHg) | HPZ-sqze (mmHg) | |
|---|---|---|---|
| Poor | 2.775 ± 0.5961 | 26 ± 11.553* | 90.57 ± 32.434* |
| Good + Fair | 2.535 ± 0.4632 | 31.22 ± 11.569 | 104.87 ± 33.089 |
| CON | 2.50 ± 0.45 | 48.89 ± 14.03 | 125.09 ± 41.21 |
Table 3.
Comparison of basic manometric parameters between good and poor functional outcomes in ARMs patients.
The difference was statistically significant vs. Good + Fair.
“Good” refers to regular bowel movement. “Fair” refers to constipation but could be solved by oral medication or laxatives, as well as occasional dirty pants occurred during sleep, cough, and diarrhea. “Poor” refers to severe constipation that bowel management (e.g., enema) was needed, whereas incontinence refers to a recurrent involuntary loss of liquid and/or solid stool in older children and frequent dirty pants in toddlers.
3.2.3 Repeated manometry in ARMs patients with defection disorders
A total of 28 patients with ARMs had more than one measurement study, and 27 of them underwent their initial measurement study between 8 and 24 months of age during routine clinical follow-up. A female patient, who underwent primary surgery at birth at a local hospital, underwent her first manometry at the age of 6 due to chronic constipation. Subsequent examinations were performed as needed, either for the purpose of re-evaluation of impaired anal function or in response to parental requests as the child grew older. The details of these patients, categorized into three groups according to their functional and initial manometric assessments, are summarized in Table 4. Patients in Group 2 were those who had good bowel behavior at the time of initial follow-up. They came back to the clinic because of episodes of bowel movement problems. This could happen at any age. In this situation, repeated measurements were conducted. Comparing with their initial measurements, some of the measurements showed values lower than the mean-SD of their age-matched controls. Further subsequent investigations (such as X-ray, contrast enema, MRI, ultrasound, and biopsy) were conducted to rule out any associated pathology. The abnormal defecation in seven patients (four with dirty pants and three with constipation) was alleviated or improved through dietary adjustments, despite some of them having lower HPZ-rest or HPZ-sqze. Patients in Group 3 who had poor or fair function at the time of initial examination were those who required further investigation and treatment. Currarino syndrome was found in two cases of low-type ARMs with constipation who underwent a simple anoplasty procedure at birth at a local hospital. During physical examination, an incorrect position of the constructed anus was identified. Additionally, strange anal canal pressure distribution with an extra length of HPZ-length was seen in one of the patients (Figure 3). After surgical removal of the tumor, soiling rather than constipation occurred, and repeated manometry was performed at the age of 2 years. Results showed that the HPZ-sqze was considerably improved compared with the initial measurement, and anal canal strength distribution was also improved although there was still significant weakness seen in the posterior quadrant during squeezing. In another case, a 6-year-old girl, who came to our clinic for an initial examination, had been suffering from chronic constipation since her primary surgery for an intermediate type of rectalvestibular fistula in early infancy. The initial manometric measurements were comparable to the mean ± SD of her age-matched group, except for a negative RAIR. In subsequent investigations, sacrococcygeal malformations were observed on X-rays, and a dilated colon was identified during contrast studies. The diagnosis of HD was confirmed through rectal biopsy, followed by treatment with a pull-through procedure. Repeated post-treatment measurements showed a slightly lower HPZ-sqze, while other measurements remain comparable to the initial ones.
| Group | Manometry | Functional outcome | Abnormal Manometric parameters | Classification of ARMS | Associated spinal/vertebral deformity | Contrast enema | Treatment | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Good | Fair | Poor | HPZ-Length | HPZ-Rest | HPZ-Sqze | RAIR (−) | Low | Inter-mediate | High/cloaca | Yes | No | Normal | Dilated Colon | Diet/Drug/Biofeed- back | Surgical | ||||
| Consti-pation | Soil-ing | SC | IC | ||||||||||||||||
| Group 1 (N = 10) | Initial | 10 | 0 | 0 | 0 | 0 | — | <(N = 2) | — | 1 | 10 | 0 | 0 | N/A | N/A | N/A | N/A | Diet (N = 4) | 0 |
| Repeated | 10 | 0 | 0 | 0 | 0 | — | <(N = 2) | — | 1 | ||||||||||
| Group 2 (N = 9) | Initial | 9 | 0 | 0 | 0 | 0 | — | — | — | 4 | 7 | 2 | 0 | 1 | 6 | 4 | 2 | Diet (N = 7) Drug (N = 1) Biofeed- back (N = 1) | Biopsy (N = 3) |
| Repeated | 0 | 3 | 5 | 0 | 1 | >(N = 1) | <(N = 6) | <(N = 3) | 3 | ||||||||||
| Group 3 (N = 9) | Initial | 0 | 5 | 3 | 0 | 1 | >(N = 1) | <(N = 2) | — | 6 | 3 | 4 | 1/1 | 3 | 6 | 5 | 4 | Diet (N = 4) Biofeed- back (N = 2) | Curra- rino (N = 2) HD (N = 1) |
| Repeated | 3 | 4 | 1 | 0 | 1 | — | <(N = 2) | <(N = 2) | 4 | ||||||||||
Table 4.
Clinical information of ARMs patients who had repeated manometric measurement.
“—" indicates the values were comparable with mean; < represents the value was lower than mean-SD; > represents the value was higher than mean + SD
SC represents severe constipation; IC represents incontinence.
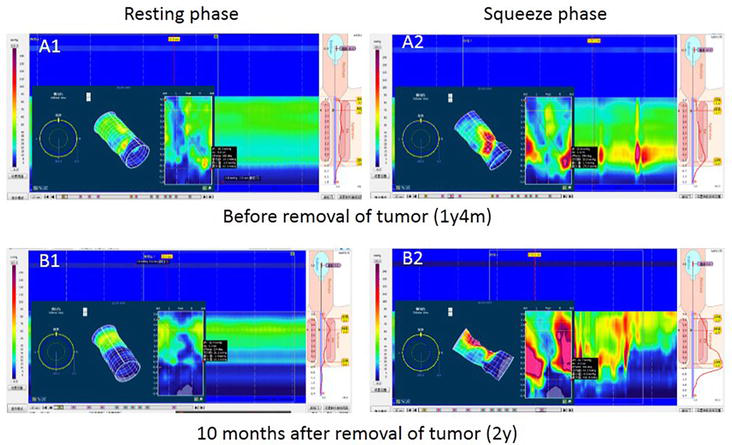
Figure 3.
3D and plane pressure maps of anal canal strength distribution in a post-operative AMRs patient associated with Currarino syndrome. A boy aged 1y4m presented with constipation and underwent primary simple ano-plasty at birth. A 6 × 5 × 3 cm anterior sacral mass (teratoma) and sacrococcygeal deformity were confirmed. Before tumor removal, an extra length of HPZ was observed in both resting (A1) and squeeze phases (A2). A manometric examination was repeated at the age of 2y (10 months after surgery) due to incontinence. The HPZ-length was comparable to the age-matched mean ± SD. Significant posterior weakness in strength distribution was observed in both resting (B1) and squeeze phases (B2).
4. Discussion
Congenital anorectal malformations are developmental defects located at the end of the digestive tract that require surgical reconstruction of the anal canal to achieve defecation. The common long-term post-operative complications include constipation and fecal incontinence [13]. The clinical scoring systems commonly used for post-operative assessment of ARMs are inadequate in accurately assessing the function of the reconstructed anal canal and its role in defecation and continence. The reason is that defecation patterns can be influenced by multiple factors involved in the mechanism.
The anorectal manometric study is essential for evaluating restorative surgical procedures of the anorectal area for both adults and children, bearing the advantages of being non-invasive, safe, and intuitive [14, 15]. The development of solid catheters with sensors has enabled precise measurement (high definition), while 3D pressure modeling provides more accurate and detailed data that can be used to assess functional disorders of the anal canal.
Several studies have utilized manometry to evaluate the post-operative anal function among patients with different types of ARMs or different surgical procedures, but none of them was done with a non-operative control group [16, 17]. During the period from infancy to childhood, both physical and anatomical development proceeds rapidly before reaching a state of maturity and stability. Therefore, it is important to learn the functional capacity of the anal canal of a normal child at the same age before assessing a reconstructed one.
Our study of 104 normal children, ranging from newborns to teenagers, showed age-dependent increases in functional anal length, resting pressure, and squeezing pressure. A gradual increase in major manometric measurements was seen until the age of 4 years, suggesting that age is a crucial factor to consider when evaluating anal canal function in early childhood. Comparing mean manometric measurements without considering the age of the ARMs patient will not yield accurate statistical results, as post-operative complications can occur at any age.
Most of the ARMs patients in our recent study [12] were routinely followed up at the scheduled time after surgery, regardless of whether they had any complications or not. The manometric parameters collected could reflect the general situation of the “neo-anus” after reconstruction surgery. The results showed a comparable HPZ-length of with the non-operative CON ones in all age-matched groups, but a significantly lower HPZ-rest.
The high-pressure zone at the distal anus is believed to be the key mechanism of fecal continence. The high pressure required for anal continence is maintained by sphincter complexes, with the internal anal sphincter (IAS) contributing approximately 50–85% of resting phase pressure, while the external sphincter (EAS) and puborectalis working coordinately during the squeeze phase. This high-pressure zone is rather a functional structure than an anatomic one, which can be measured by the algorithm of analysis software and presented as the length of the area where the resting anal pressures exceed the resting intrarectal pressure by at least 5 mmHg in manometry. With this understanding, it is not difficult to explain our results in ARMs patients. However, significantly lower HPZ-rest values were observed in the majority of patients with incontinence ARMs compared to those with continence ARMs, indicating weak or degenerated IAS, regardless of whether this was due to poor primary development or damage from surgical dissection.
The external sphincter is a voluntary striated muscle that completely surrounds the anal canal and rectum and is divided into subcutaneous, superficial, and deep parts through the longitudinal and anal levator ani fibers. The HPZ-sqze is an indicator of voluntary contractions resulting from coordinate contractions in the unique triple-looped anatomy of the EAS complex and puborectalis. Any type of anal reconstructive surgery has the potential to affect local muscles and nerves. The selection of a surgical procedure should be based on the surgeon’s experience in dealing with patients with different classifications of ARMs. One of the key steps is to place in the end of the rectum at the correct anatomical position so that it would be surrounded by the muscle complex. Statistical analysis of our study shows that functional outcomes were only correlated with the classification of the ARMs, not with surgical approaches. This indicates that the optimal functional outcome can be achieved with meticulous manipulation. If the effects of surgical manipulation are excluded, the underdeveloped anorectal structures, including sphincter muscle complexes and neural networks, seen more frequently in patients with high-type ARMs and cloacae, may be a major cause of inadequate functional outcomes. Conversely, factors other than abnormal embryonic development of the sphincter and nervous system should be considered in patients with ARMs who are not classified as high type but who claim incontinence. Extensive dissection or rough manipulation during surgery might result in damage to local muscles and nerves, while the incorrect placement of the anal canal would result in the risk of a newly reconstructed anus not properly surrounded by EAS.
With 3D models, asymmetry strength distribution of the anal canal was also seen in the non-operative CON as what has been observed in adults [18]. The reason for this may be attributed to the uneven development of different muscles leading to unbalanced sphincter complex response for maintaining the high pressure zone. In patients with ARMs, hypo-development of the anal sphincter complex in different degrees is common and may alter the pressure distribution. Image studies, such as MRI [19] and ultrasound [20], are recommended to identify the development of muscle complex and the location of the neo-anus in order to determine whether weakness is due to poor development or incorrect placement of the anal canal.
The mechanisms of RAIR and the neural pathways of reflex have remained unknown, though its prominent role in normal defecation and sensation is believed to depend upon the intrinsic intramural nerve network regulated by the sacral medullary [21]. A recent systematic review [22] concluded that the absence of RAIR indicated low quality or damage of the IAS, which might be due to poorly developed anorectal structures in ARMs patients with poor continence. In our series of ARMs studies, a higher incidence of negative RAIR and significantly lower HPZ-rest in the incontinence ARMs patients suggested poor sensation and weakness of their IASs. Negative RAIR is usually associated with an HD diagnosis. Although the coexistence of ARMs and HD is rare, accounting for only about 2% in ARMs patients according to a previous study [23], it is still necessary to rule out HD via biopsy, as reminded in our study in which one case of such combined symptoms was identified.
In a previous study [24] that compared four different scoring systems (Holschneider’s, Rintala’s, Krickenbeck’s, and Peña’s Questionnaires) based on anorectal manometry measurements, it was recommended that Holschneider’s and Rintala’s questionnaires be used in patients’ follow-up, while Peña’s and Krickenbeck’s questionnaires in determining a proper bowel management program for patients rather than patients’ follow up. Up to now, there is no widely accepted method for assessing the follow-up of patients with ARMs. Although it is difficult to identify the reasons for bowel functional outcomes using independent scoring systems, evaluations using questionnaires and scoring systems are certainly the first step. General information about bowel movement patterns should be collected ahead of any anorectal manometry. Very likely, patients or their parents may overstate the severity of “poor bowel functions” when completing a questionnaire. Therefore, it is important to ask detailed questions, such as daily diets (including any special food that may induce either constipation or soiling), medications taken, and other situations that may affect bowel movements. After a physical examination and clinical assessment, manometry and necessary radiographic studies should be performed to rule out other associated birth defects (spinal malformation or Currarino syndrome), and sometimes even a biopsy should be run to exclude HD. One fecal incontinence patient had comparable anorectal manometric parameters with her age-matched ARMs patients who having “Good and Fair” functional outcomes. Using this diagnostic algorithm, an infectious rectovestibular fistula was eventually diagnosed through careful physical examination, ultrasound, and contrast enema studies.
Conservative treatment is initially recommended for individuals with poor manometric measurements, which may include dietary fiber supplementation, stool modification drugs, biofeedback physiotherapy, trans-anal irrigation, or a combination of these interventions. After a certain period of treatment (at least 3 months), a subsequent manometric examination is conducted to assess the potential improvements in comparison with the previously measured parameters.
Fecal continence may be affected by extrinsic factors beyond the anorectum. The regulation and control of defecation (continence) depend upon the interaction between local anatomical structures, such as anorectum and pelvic floor musculature, and physiological systems, primarily involving nerves and cognitive. However, our current study is limited by the fact that most of our ARMs patients were relatively young, and only a few patients were able to complete such tests as defecation perception and simulated defecation.
Although anorectal manometry is now the most widely used investigational tool for detecting abnormalities in anorectal coordination and/or anal sphincter complex dysfunction, as stated in a recent systematic review on anorectal manometry in children who have undergone ARMs repair, it remains clinically challenging to determine the definitive thresholds for sphincter dysfunction that may lead to fecal incontinence [25].
According to their systematic review [25], manometric studies have been performed for the purpose of comparing different types of ARMs, evaluating operative techniques, assessing post-operative modalities, predicting bowel function, and investigating the pathophysiology and management of post-operative bowel dysfunction. Different manometric equipment, assessment protocols, and parameter definitions used in various studies have led to significant deviation in results. For example, in the efforts to identify abnormalities in anorectal function, what is considered “normal” was rarely provided or described in a clear definition. This makes it difficult to interpret the findings and compare data between different studies. Our current studies were based upon the understanding of the “normal” pediatric physiology, and such a criterion was held persistently from the design stage until post-operative determination of abnormalities. We recommend using the same measurement equipment or the same model and standardization procedure and having the same team collect and analyze the data to minimize confounding factors. In addition, the collection of manometry parameters of non-operative CON to establish a “normal” reference for future assessment of patients who may undergo any kind of anorectal surgeries and further prognostic training and evaluation. There is no need for frequent manometric studies in patients who underwent an anorectal surgery during early infancy, but even in the absence of any complications, one single manometric exam between the ages of 18–24 months is recommended. Within the first year of toddlerhood, the rapid physical development of the anal rectum is complete and the transition from formula to a solid food diet has been completed, making them ready for toilet training. Such a manometric record will provide basic information on the individuals with reconstructed anal canal in case of later occurrence of defecation disorder, since it may happen at any age (Figure 4). For those who have poor anal function, a long-term follow-up is necessary as the defecation problems may persist into adolescent or even adulthood. Therapeutic strategies should be carefully considered together with manometric findings. Manometric records provide valuable information regarding the actual origin of continence problems that may not always be clinically distinguished.
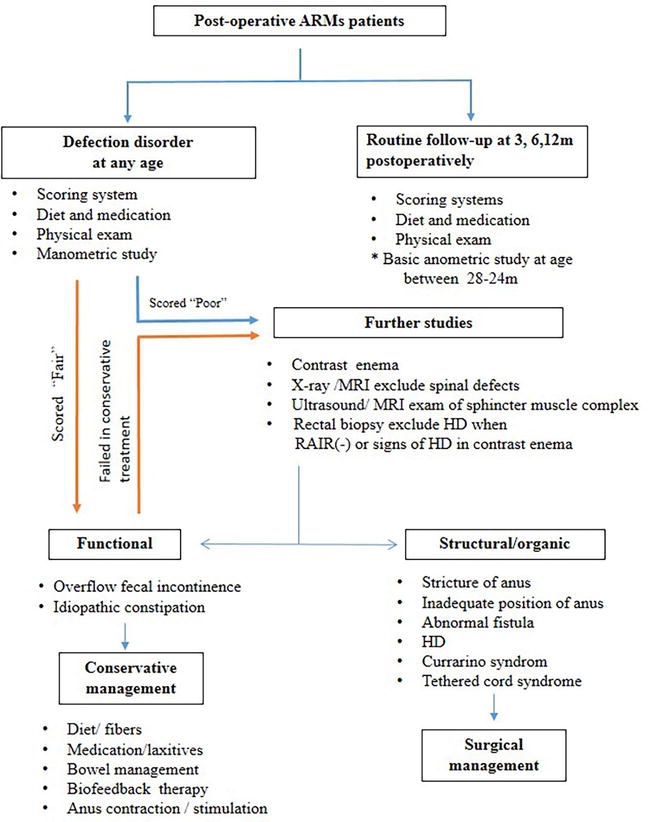
Figure 4.
An algorithm presenting the proposed pathway for assessment of post-operative anal function. Routine follow-up at the outpatient clinic is recommended at 3, 6, 12 months after the operation. * One single manometric exam between 18 and 24 months of age is recommended to collect basic parameters of the anal canal even in the absence of any complications. Once defecation disorder occurs, patients classified as “Fair” with normal manometric results may be considered as having a functional disorder and initially managed with conservative treatment. Patients classified as “Poor”, as well as those who failed with conservative treatment should undergo further investigations to exclude other associated disease or surgery-related structural problems.
5. Conclusions
To conclude our study, age should be considered as an essential factor when evaluating post-operative anorectal function in ARMs patients. Classification of high-type and cloaca in ARMs and low HPZ-rest are two factors that affect post-operative functional outcomes. Different operative procedures or approaches do not affect the functional outcomes. 3D high-definition manometry is a valuable modality to provide accurate details of anal function based on age-matched non-operative CON in early childhood. The proper assessment will provide physicians with information on potential causes of complications, meanwhile, it will also provide the guidelines for the selection of adequate treatment modalities.
Acknowledgments
No funding was received to support this study. Weihong Guo designed the research study; Jiawei Zhao, Yanan Zhang, Yu Xiong, and Weihong Guo performed the research; Yanan Zhang, Weihong Guo interpreted data; Jiawei Zhao, Weihong Guo analyzed the data and wrote the paper.
Abbreviations
anorectal malformations | |
anorectal high-pressure zone | |
the length of HPZ | |
the mean resting pressure of HPZ | |
the mean squeeze pressure of HPZ | |
recto-anal inhibitory reflex | |
Hirschsprung’s disease | |
internal anal sphincter | |
external anal sphincter |
References
- 1.
Yuan P, Qiao L, Dai L, et al. Spatial distribution patterns of anorectal atresia/stenosis in China: Use of two-dimensional graph-theoretical clustering. World Journal of Gastroenterology. 2009; 15 :2787-2793. DOI: 10.3748/wjg.15.2787 - 2.
Nah SA, Ong CCP, Safari SE, et al. Anorectal malformation & Hirschsprung’s disease: A cross-sectional comparison of quality of life and bowel function to healthy controls. Journal of Pediatric Surgery. 2018; 53 :1550-1554. DOI: 10.1016/j.jpedsurg.2017.08.018 - 3.
Rintala R, Mildh L, Lindahl H. Fecal continence and quality of life for adult patients with an operated high or intermediate anorectal malformation. Journal of Pediatric Surgery. 1994; 29 :777-780. DOI: 10.1016/0022-3468(94)90368-9 - 4.
Holschneider A, Hutson J, Peña A, et al. Preliminary report on the international conference for the development of standards for the treatment of anorectal malformations. Journal of Pediatric Surgery. 2005; 40 :1521-1526. DOI: 10.1016/j.jpedsurg.2005.08.002 - 5.
Carrington E, Knowles C, Grossi U, Scott S. High-resolution anorectal manometry measures are more accurate than conventional measures in detecting anal hypocontractility in women with fecal incontinence. Clinical Gastroenterology and Hepatology. 2019; 17 :477-485.e479. DOI: 10.1016/j.cgh.2018.06.037 - 6.
Ambartsumyan L, Shaffer M, Carlin K, Nurko S. Comparison of longitudinal and radial characteristics of intra-anal pressures using 3D high-definition anorectal manometry between children with anoretal malformations and functional constipation. Neurogastroenterology and Motility. 2021; 33 :e13971. DOI: 10.1111/nmo.13971 - 7.
Zhao J, Zhang Y, Xiong Y, et al. Three dimension high-definition manometry in evaluation of anorectal function in 104 normal infants and children: A clinical study from China. Neurogastroenterology and Motility. 2022; 34 :e14395. DOI: 10.1111/nmo.14395 - 8.
Kumar S, Ramadan S, Gupta V, et al. Manometric tests of anorectal function in 90 healthy children: A clinical study from Kuwait. Journal of Pediatric Surgery. 2009; 44 :1786-1790. DOI: 10.1016/j.jpedsurg.2009.01.008 - 9.
Baaleman D, Velasco-Benítez C, Méndez-Guzmán L, Benninga M, Saps M. Functional gastrointestinal disorders in children: Agreement between Rome III and Rome IV diagnoses. European Journal of Pediatrics. 2021; 180 :2297-2303. DOI: 10.1007/s00431-021-04013-2 - 10.
Stephens F. Wingspread anomalies, rarities, and super rarities of the anorectum and cloaca. Birth Defects Original Article Series. 1988; 24 :581-585 - 11.
Wood R, Levitt M. Anorectal malformations. Clinics in Colon and Rectal Surgery. 2018; 31 :61-70. DOI: 10.1055/s-0037-1609020 - 12.
Divarci E, Ergun O. General complications after surgery for anorectal malformations. Pediatric Surgery International. 2020; 36 :431-445. DOI: 10.1007/s00383-020-04629-9 - 13.
Carrington E, Brokjaer A, Craven H, et al. Traditional measures of normal anal sphincter function using high-resolution anorectal manometry (HRAM) in 115 healthy volunteers. Neurogastroenterology and Motility. 2014; 26 :625-635. DOI: 10.1111/nmo.12307 - 14.
Banasiuk M, Banaszkiewicz A, Piotrowski D, et al. 3D high-definition manometry in evaluation of children after surgery for Hirschsprung’s disease: A pilot study. Advances in Medical Sciences. 2016; 61 :18-22. DOI: 10.1016/j.advms.2015.07.008 - 15.
Brisighelli G, Macchini F, Consonni D, et al. Continence after posterior sagittal anorectoplasty for anorectal malformations: Comparison of different scores. Journal of Pediatric Surgery. 2018; 53 :1727-1733. DOI: 10.1016/j.jpedsurg.2017.12.020 - 16.
Bjørsum-Meyer T, Christensen P, Jakobsen M, Baatrup G, Qvist N. Correlation of anorectal manometry measures to severity of fecal incontinence in patients with anorectal malformations - A cross-sectional study. Scientific Reports. 2020; 10 :6016. DOI: 10.1038/s41598-020-62908-w - 17.
Azpiroz F, Enck P, Whitehead WE. Anorectal functional testing: Review of collective experience. The American Journal of Gastroenterology. 2002; 97 :232-240. DOI: 10.1111/j.1572-0241.2002.05450.x - 18.
Li Y, Yang X, Xu C, Zhang Y, Zhang X. Normal values and pressure morphology for three-dimensional high-resolution anorectal manometry of asymptomatic adults: A study in 110 subjects. International Journal of Colorectal Disease. 2013; 28 :1161-1168. DOI: 10.1007/s00384-013-1706-9 - 19.
Gangopadhyay A, Pandey V, Gupta D, et al. Assessment and comparison of fecal continence in children following primary posterior sagittal anorectoplasty and abdominoperineal pull through for anorectal anomaly using clinical scoring and MRI. Journal of Pediatric Surgery. 2016; 51 :430-434. DOI: 10.1016/j.jpedsurg.2015.09.003 - 20.
Wang Z, Hu L, Jin X, Li X, Xu L. Evaluation of postoperative anal functions using endoanal ultrasonography and anorectal manometry in children with congenital anorectal malformations. Journal of Pediatric Surgery. 2016; 51 :416-420. DOI: 10.1016/j.jpedsurg.2015.09.024 - 21.
Espinosa-Medina I, Saha O, Boismoreau F, et al. The sacral autonomic outflow is sympathetic. Science. 2016; 354 :893-897. DOI: 10.1126/science.aah5454 - 22.
Rajasegaran S, Tan W, Ezrien D, et al. Utility of postoperative anorectal manometry in children with anorectal malformation: A systematic review. Pediatric Surgery International. 2022; 38 :1089-1097. DOI: 10.1007/s00383-022-05152-9 - 23.
Nakamura H, Puri P. Concurrent Hirschsprung’s disease and anorectal malformation: A systematic review. Pediatric Surgery International. 2020; 36 :21-24. DOI: 10.1007/s00383-019-04580-4 - 24.
Mert M, Sayan A, Köylüoğlu G. Comparing the fecal continence scores of patients with anorectal malformation with anorectal manometric findings. Pediatric Surgery International. 2021; 37 :1013-1019. DOI: 10.1007/s00383-021-04884-4 - 25.
Evans-Barns HME, Tien MY, Trajanovska M, et al. Post-operative anorectal manometry in children following anorectal malformation repair: A systematic review. Journal of Clinical Medicine. 2023; 12 (7):2543. DOI: 10.3390/jcm12072543