Abstract
The aim of this study is to determine the effectiveness of COBLATION midline glossectomy for obstructive sleep apnea (OSA) when used as an isolated or with palatal procedure. We also aim to compare the effect of this surgical procedure. The combination of palatal procedures and tongue-based surgery in a single stage led to improvement in excessive daytime sleepiness, snoring, respiratory parameters of polysomnography (PSG), an overall improvement in quality of life, we can show how de tongue base procedures with COBLATION can give better results to all sleep apnea surgeries. Currently, there is a wide variety of surgical approaches to tongue-base modification in OSA patients, including radiofrequency ablation, COBLATION or laser assisted resection, tongue base suspension, genioglossus advancement, and robot-assisted resection. COBLATION midline glossectomy is an effective surgical procedure.
Keywords
- coblation
- midline glossectomy
- OSA
- tongue base surgery
- snore
1. Introduction
Obstructive sleep apnea (OSA), is a disease that leads to recurrent episodes of upper airway obstruction, which can lead to partial or complete obstruction of the upper airway, it is a chronic and progressive condition [1]. OSA causes excessive daytime sleepiness, and brings many adverse consequences, such as hypertension, obesity, diabetes mellitus, cardiac and encephalic alterations, depression e anxiety, irritability, diminuiçao da libido is a public health problem and studies show that today it affects approximately 30% of the world’s population [2].
Continuous positive airway pressure (CPAP) devices are traditionally used as the standard treatment for OSA; however, patient compliance with the treatment is low, and non-compliant patients are commonly considered candidates for surgical treatment [3, 4]. Usually the levels of obstruction are usually different from one patient to the next; Therefore, the appropriate surgical procedure should be evaluated for each case, in this the topographic diagnosis is fundamental for surgical success. The surgery will only be successful if the diagnosis and the sites of obstruction have been well established, only then we can compare the success of each surgical technique and choose the one that best suits the patient, according to the particularity of each patient.
There are numerous, procedures directed to specific sites of the airway and widely disseminated to treat obstructive sleep apnea (OSA), one of them and what we cover extensively in this chapter is the glossectomy of the midline, a procedure that acts directly by amplifying the hypopharyngeal airspace, Fujita in 1991, described the tongue base procedure using the carbon dioxide laser and stars a new era in tongue base surgery access [5].
As previously stated, several surgeries aim to tackle different sites of upper airway obstruction, each with its particularity and always taking into account the treatment of obstructive sleep apnea. We can consider that the palate and the base of the tongue are the most common targets of OSAS surgery, and the resection of the base of the tongue with COBLATION has been proposed and has become the target of numerous studies due to the great efficacy that has been presented; The positive results and the low level of complications speak in favor of this type of approach. Given this idea, we observed that the approach of several surgical sites in the same step and surgical moment is the golden surgery for the treatment of sleep apnea.
The tongue base surgery with COBLATION, can be associated with any procedure related to the treatment of OSA, the maxillomandibular advancement for example, can have immense benefit when we use the association of COBLATION, since we can perform a smaller advance, reducing craniofacial changes, postoperative morbidities, dysfunctions of the temporo-mandibular joint and reducing the index of sleep apnea and hypopnea drastically, with improvement in the patient’s quality of life.
2. COBLATION what is that?
COBLATION means ‘Controlled Ablation’. COBLATION Technology uses a plasma field to precisely dissolve targeted tissue while maintaining the integrity of surrounding tissue. Unlike radiofrequency-based devices that use high temperatures to cut and cauterize, COBLATION Technology uses lower temperatures causing minimal damage to surrounding tissue [6].
A range of COBLATION Wands are designed for both tonsil and adenoid procedures, with integrated saline delivery and suction, and malleable shafts. In our procedures we use the tip PROCISE MAX, designed for surgeons who prefer rapid tissue removal in his procedures with low thermal effect and easily during hemostasis, since the device itself allows us to use the ablation and coagulation function, the system is integrated with suction and with distillation of saline solution, that reduces thermal effect and assists suction, is an all-in-one instrument designed to help decrease surgical time and avoid some complications.
3. Access to the tongue base
In fact, there is a wide variety of surgical approaches for partial reduction of the base of the tongue for patients with sleep apnea, including radiofrequency ablation, COBLATION or laser assisted resection, tongue base suspension, genioglossus advancement, and transoral robotic surgery (TORS) [7]. We have not yet found the ideal treatment technique, even with the evidence of high success rates, on the other hand, there are studies that show high variability of these rates, which makes it even more difficult to adhere to the ideal technique for this complex and challenging disease. We always provide surgery in associated with palatal techniques because we believe that in this way in addition to reducing the rate of sleep apnea and hypopnea above the expected, we will also have the reduction of snoring.
We began the procedure by performing dexmedetomidine induced sonoendoscopy, where we evaluate airway collapse at different levels improving surgical accuracy and definition, drug induced sleep endoscopy (DISE), usually takes 15 min [8] reaching only N2 sleep. However, it is during this phase that most events occur, we believe that this short period of time can already show us a large part of what happens during the patient’s night, in the ideal world we should spend the night next to this patient and perform the nasofibroscopy during natural sleep. Therefore, DISE, despite not providing all obstructive events that occur in the patient, is an extremely effective tool, easy to apply and which often leads us to realize that we have missed some point of obstruction during the assessment in the office, where we perform the muller maneuver, which today we know how limited it is. After careful visualization of the obstructive surgical sites, we performed traction of the tongue and suture it in the surgical field, to improve exposure of the base of the tongue.
A 30° optics is used to assist in the visualization of the base of the tongue, we use the COBLATION in ablation mode, where there is a rapid tissue removal while maintaining the hemostatic and minimal thermal effect benefits (Figure 1A and B), so without deepening the ablation by the risk of injury of noble structures of the base of the tongue such as the lingual artery, the ideal would be to evaluate the distance from the surface of the tongue to the hypoglossal/lingual artery neurovascular bundle to constant surface landmarks in the base of tongue during surgically simulated retraction versus resting anatomic position (Figure 2), so that we can with tranquility carry out the dissection of this tissue without produce injurys [9, 10].
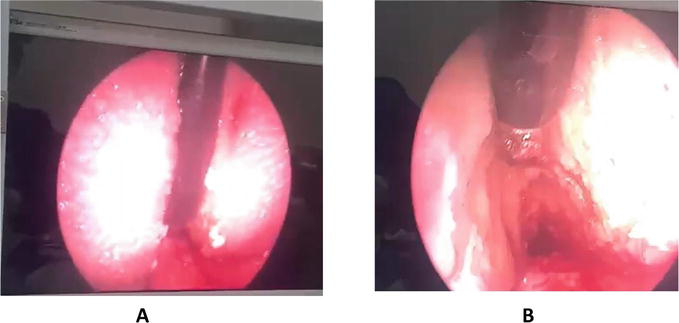
Figure 1.
A. Note the work of coblation wands, at the base of the tongue, always in the midline, B. then already during the partial ablation of the base of the tongue we see much of the tongue tissue removed showing an expressive reduction of the base of the tongue.
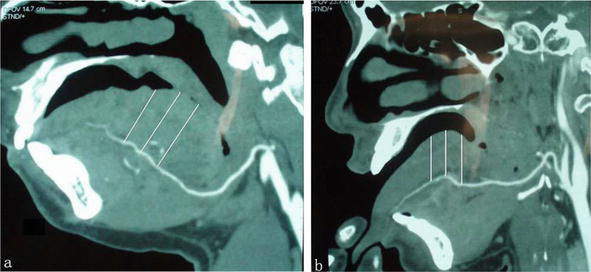
Figure 2.
Sagital views of computed tomography scan of a patient with obstructive sleep apnea syndrome the lingual artery in the resting position (a) and during the extension position of the way we perform the surgical procedure (b). The length of the white line indicates the depths of the lingual artery beneath the lingual surface based on three reference marks.
Soon after the end of the ablation we perform the coagulation of bleeding points of the base of the tongue with the COBLATION itself, which has this option during the procedure, the coagulations should be punctual and should not extend to the lateral redundant tissue of the base of the tongue, we also know that there is no correct amount of lingual tissue to be removed, This depends on the previous characteristics evaluated preoperatively and in sonoendoscopy, which show how bulky this tongue base is and how much it occupies the anteroposterior airspace.
After the procedure of the base of the tongue is finished, we continue the multilevel surgery, using palatal techniques and nasal surgeries in most cases, and at the end of the whole procedure we performed the review of coagulation and intraoperative edema that can be caused, usually insignificant in our point of view, patients are extubated and taken to the recovery room without the need for intensive care, but with hospitalization of at least 1 day for evaluation of ventilatory parameters and prevention of possible bleeding.
4. Complications
Postoperative pain and submandibular edema were 2 most common postoperative complications which can be easily controlled by antibiotics, [11] the most common intraoperative complication is bleeding, already during the postoperative period we have hematoma, edema, abscess, taste changes, reduced mobility of the base of the tongue, temporary dysphagia, changes during swallowing, paresthesia, usually all reversible after a few months of the procedure and with easy management in the office, This patient should be followed for at least 1 year with careful evaluations and nasofibrolaryngoscopy.
The most feared complication of surgery is velopharyngeal stenosis, which occurs due to excessive removal of the base of the tongue outside the midline when associated with palatal surgeries, a complication that leads to reduced quality of life of the patient as well as respiratory disorders (Figure 3).

Figure 3.
Patient in 4 months after surgery of lateral expansion pharyngoplasty, midline glossectomy with COBLATION, turbinectomy and septoplasty, we see fibrous scar tissue stenosing the airway and maintaining small respiratory pertuito through the oropharynx.
Just to know, this patient was treated with a new surgery of expansion and lateralization of the palate with important improvement, but with maintenance of fibrotic tissue, in the future probably should be submitted to new palatal expansion, and application of local anti-inflammatory medication.
5. Role of the base of the tongue in sleep apnea
Glossectomy significantly improves sleep outcomes as part of multilevel surgery in adult patients with OSA [12]. The studies have already shown the surgical efficacy both alone and in multilevel surgeries, when there is a careful selection of patients and a good indication the surgery has an important response in the treatment of sleep apnea.
In our sample of 28 operated patients, all in surgeries combined with midline glossectomy with COBLATION, expansive lateral pharyngoplasty, septoplasty and turbinectomy, we verified a significant improvement in the evaluation of the epworth sleep scale from 13 ± 9.4 preoperatively to 3.1 ± 2.4 postoperatively, the visual score analogue mean score of preoperative snoring ranged from 7.8 ± 4.1 to 3.1 ± 1.5 postoperatively.
And when we talk about the sleep apnea and hypopnea index (AHI), we show a significant reduction from 26.3 ± 28.2 to 10.4 ± 16.2 in the postoperative period.
The technique of partial glossectomy for the treatment of OSA has been described for some time, today we can present numerous techniques with varying degrees of efficacy, all these procedures are based on the attempt to partially remove the base of the tongue or its redundant tissue. Sleep surgeries that fit this criterion include midline glossectomy (MLG), submucosal minimally invasive lingual excision (SMILE), and lingualplasty (LP). Fujita was the first to describe removal of tongue tissue for OSA with the MLG [5].
We believe that tongue-based surgery, isolated is effective, brings benefit of sleep apnea, but we know that for us to have a better reduction of AHI, the surgery combines multilevel is certainly more effective.
A recent review about the new treatments for OSA, they try to affirm that midline glossectomy is not a good option and cases of moderate sleep apnea, especially in obese people, obviously believe that when there is a body mass index above 40 kg/m2, no surgical alternative is coherent, and the first step should be weight loss [13]. The evidence we present does not disagree with this statement, but when there is a correct surgical indication seen the patient as a whole, as well as the topographic evaluation evidencing that the base of the tongue is the problem in question, glossectomy alone can become a strong ally and can be effective in the treatment of OSA.
6. What we can expect from tongue-base surgeries
Surgeries that access the base of the tongue have evolved significantly in recent years, with the advent of robotic surgery transoral robotic surgery (TORS), and hypoglossal nerve stimulator.
Vicini et al. demonstrated, the condition presented in the hypertrophy of the base of the tongue, is a difficult management, the surgery to remove the accentuated hypertrophy of the base of the tongue, is a challenge for both the patient and the surgeon, so the studies are increasingly in search of the perfect surgery for this structure [14].
The robotic setup, which permits multiplanar tissue transection at any angle, enhances the surgeon’s dissecting skills in such a complex anatomical region, and, as opposed to traditional open approaches, tongue base resection by means of TORS seems to be very well tolerated.
On the other hand, and talking about another type of surgery, one of the most recent treatments for OSA and that has shown efficacy is the hypoglossal nerve stimulator, is a device that generates electrical impulses through a generator that is implanted in the upper right chest (under the skin). The electrical impulse is transmitted directly to the hypoglossal nerve. Today we have in the market three devices being tested in clinical trials, with publications in the most important otorhinolaryngology journals in the world. The Apnex Medical Inc. (St. Paul, MN, USA) device was promising in a phase II trial but failed at phase III because it did not meet efficacy standards and the company does not exist now (Figure 4). The second device is the ImThera aura 6000 (San Diego, CA, USA). It places six electrodes around the trunk of the hypoglossal nerve. It is still in phase III clinical trial (Figure 5). The third device, which is the only one approved by the FDA, is Inspire Medical Systems (Maple Grove, MN, USA) (Figure 6). Since it is the only one approved by the FDA, so we believe that future medical literature papers about hypoglossal neurostimulators will be based directly on Inspire medical Systems [15].
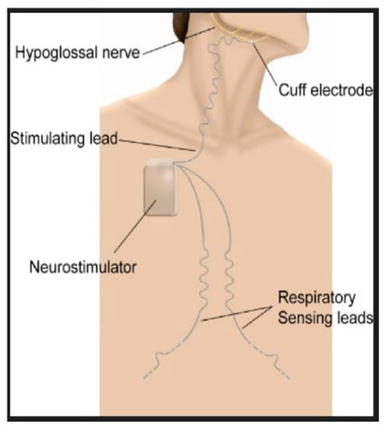
Figure 4.
Apnex Medical Inc. (St. Paul, MN, USA).
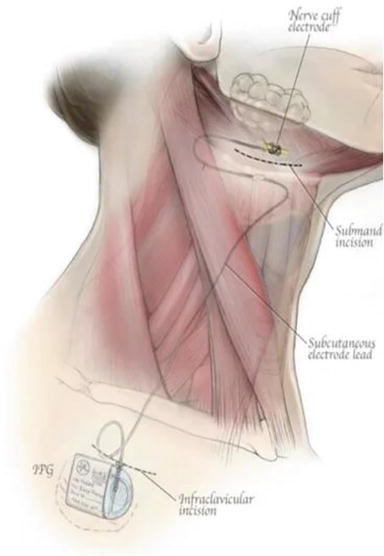
Figure 5.
ImThera aura6000 (San Diego, CA, USA).

Figure 6.
The Inspire system (Maple Grove, MN, USA).
7. Final considerations
Snoring is extremely common in the general population and when irregular may indicate a predisposing to sleep apnea [16].
The combination of palatal procedures with tongue-based surgery in a single stage, lead to improvement of excessive daytime sleepiness, snoring, respiratory parameters of polysomnography, an overall improvement in quality of life. The results presented in the literature favor the application of the combined procedure, even knowing that the tongue base treated alone is effective, thus contributing as another therapeutic option in obstructive sleep apnea.
It is important to emphasize that the more we study the neurophysiology of the complex syndrome of obstructive sleep apnea, the more we come across studies indicating the basis of the tongue as a problem and the surgery of the same as a resolution even if temporary of the disorders related to sleep apnea, I believe that the evolution within the tongue-based surgeries as well as the understanding of the functionality of the same within this wonderful world that is the knowledge of the syndrome itself brings us easier and easier paths with less morbidity and with increasingly satisfactory results.
During these years of experience and in my view the surgery performed with the COBLATION has easy applicability and extremely favorable results compared to other types of accesses to the base of the tongue. Evolution is imminent and we will work so that the future shows us more and more conditions to cure this complex disease that is obstructive sleep apnea.
References
- 1.
Park JG, Ramar K, Olson EJ. Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clinic Proceedings. Jun 2011; 86 (6):549-554; quiz 554-5. doi: 10.4065/mcp.2010.0810. PMID: 21628617; PMCID: PMC3104914 - 2.
Pinto JA, Ribeiro DK, Cavallini AF, Duarte C, Freitas GS. Comorbidities associated with obstructive sleep apnea: A retrospective study. International Achieves of Otorhinolaryngology. 2016; 20 (2):145-150. DOI: 10.1055/s-0036-1579546 - 3.
Weaver TE, Maislin G, Dinges DF, Bloxham T, George CFP, Greenberg H. Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep. 2007; 30 :711-719 - 4.
Engleman HM, Martin SE, Douglas NJ. Compliance with CPAP therapy in patients with the sleep apnea/hypopnoea syndrome. Thorax. 1994; 49 :263-266 - 5.
Fujita S, Woodson BT, Clark JL, Wittig R. Laser midline glossectomy as a treatment for obstructive sleep apnea. The Laryngoscope. 1991; 101 :805-809 - 6.
Stadler KR. Electrosurgical plasmas. Journal of Physics D: Applied Physics. 2005; 38 :1728-1738 - 7.
Kezirian EJ, Goldberg AN. Hypopharyngeal surgery in obstructive sleep apnea: An evidence-based medicine review. Archives of Otolaryngology – Head & Neck Surgery. 2006; 132 (2):206-213 - 8.
Carrasco Llatas M, Agostini Porras G, Cuesta González MT, Rodrigo Sanbartolomé A, Giner Bayarri P, Gómez-Pajares F, et al. Drug-induced sleep endoscopy: A two drug comparison and simultaneous polysomnography. European Archives of Oto-Rhino-Laryngology. 2014; 271 (1):181-187. DOI: 10.1007/s00405-013-2548-3 - 9.
Cohen DS, Low GMI, Melkane AE, Mutchnick SA, Waxman JA, Patel S, et al. Establishing a danger zone: An anatomic study of the lingual artery in base of tongue surgery. The Laryngoscope. 2017; 127 :110-115. DOI: 10.1002/lary.26048 - 10.
Wu D, Qin J, Guo X, Li S. Analysis of the difference in the course of the lingual arteries caused by tongue position change. The Laryngoscope. 2015; 125 :762-766. DOI: 10.1002/lary.24959 - 11.
Chen JH, Luo ZH, Xu HX, Yang XL, Zhu MW, Tao ZZ. Complications of tongue base reduction with radiofrequency tissue ablation on obstructive sleep apnea hypopnea syndrome. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2010; 45 (7):574-577 - 12.
Murphey AW, Kandl JA, Nguyen SA, Weber AC, Gillespie MB. The effect of Glossectomy for obstructive sleep Apnea: A systematic review and Meta-analysis. Otolaryngology and Head and Neck Surgery. 2015; 153 (3):334-342. DOI: 10.1177/0194599815594347 - 13.
Keymel S, Kelm M, Randerath WJ. Non-CPAP therapies in obstructive sleep apnoea: An overview. Pneumologie. 2013; 67 :50-57 - 14.
Vicini C, Dallan I, Canzi P, Frassineti S, La Pietra MG, Montevecchi F. Transoral robotic tongue base resection in obstructive sleep apnoea-hypopnoea syndrome: A preliminary report. ORL: Journal for Otorhinolaryngology and Its Related Specialties. 2010; 72 (1):22-27. DOI: 10.1159/000284352 - 15.
Mashaqi S, Patel SI, Combs D, Estep L, Helmick S, Machamer J, et al. The hypoglossal nerve stimulation as a novel therapy for treating obstructive sleep Apnea—A literature review. International Journal of Environmental Research and Public Health. 2021; 18 :1642. DOI: 10.3390/ijerph18041642 - 16.
Alencar AM, Vaz DG, da Silva C, Oliveira B, Vieira AP, Moriya HT, et al. Dynamics of snoring sounds and its connection with obstructive sleep apnea. Physica A: Statistical Mechanics and its Applications. 2013; 392 (1):271-277