Abstract
Throughout this chapter, we will discuss the treatment of greater tuberosity fractures of the proximal humerus. Greater tuberosity fractures are common, and an increase is expected due to population aging. We can address these fractures in different ways to restore the anatomy and function of the patient, but surgery is usually selected for displaced fractures. The surgical approach remains unclear, and few data can guide surgeons in choosing one technique or another. We will discuss open versus less invasive and arthroscopic repair techniques for fractures of the greater tuberosity of the humerus, and we will try to underline the advantages and cons of each method and describe the evidence around each surgical technique. We will also include some tips and tricks that may be helpful to orthopedic surgeons to achieve an optimal outcome.
Keywords
- arthroscopy
- greater tuberosity fractures
- shoulder
- double-row suture
- proximal humerus
1. Introduction
Isolated, more significant tuberosity fractures account for up to 20% of all proximal humeral fractures [1, 2, 3]. Proximal humerus fractures are more common in elderly female patients with poor bone quality following low-energy trauma. Women are affected three times more often than men. In contrast, in younger patients, greater tuberosity (GT) fractures usually occur in males following high-velocity trauma [4].
The proximal humerus, a critical upper limb component, possesses intricate anatomical, osteomuscular, vascular, and nervous structures that collectively contribute to its functionality and clinical significance. This region encompasses the humeral head, anatomical neck, greater and lesser tubercles, and adjacent soft tissues, all intricately interacting to enable a wide range of upper limb movements and maintain shoulder stability. A comprehensive understanding of the proximal humerus’s osteomuscular, vascular, and nervous anatomy is essential for medical professionals involved in clinical assessment, surgical interventions, and rehabilitative strategies.
Numerous studies have explored the multifaceted anatomy of the proximal humerus. Anatomically, the humeral head articulates with the glenoid fossa of the scapula, forming the glenohumeral joint. This complex joint relies on a delicate balance of osteological structures, such as the articular surfaces and the anatomical neck, to ensure joint congruency and proper movement mechanics. Meanwhile, the greater and lesser tubercles are attachment sites for vital muscles, including the rotator cuff, contributing to the intricate dynamics of shoulder movement and stability.
Vascular supply to the proximal humerus is a vital aspect often explored in anatomical and clinical literature. Studies by Le Minor et al. [5] highlight the branching patterns of the humeral circumflex arteries, which are essential for nourishing the bone and surrounding tissues. A crucial aspect often investigated in anatomical studies is vascular supply to the greater tuberosity. Research by Iacobellis et al. [6] and Basat et al. [7] elucidates the vascularization patterns of the humeral tuberosities, including the trochiter, through angiographic studies. Understanding the blood supply to this region is crucial for surgical procedures involving the proximal humerus, as compromised blood flow can impact bone healing and tissue recovery.
The intricate neural network within the proximal humerus region has been extensively studied. Research by Standring et al. [8] emphasizes the role of the axillary and suprascapular nerves in innervating the muscles and transmitting sensory information from the shoulder region. Understanding nerve pathways is crucial in clinical settings to diagnose nerve-related issues, especially posttraumatic or iatrogenic injuries.
One must account for the forces that cause deformation due to the contraction of the rotator cuff (RC) muscles when deciding on the best surgical fixation approach for fractures involving the greater tubercle (GT). The supraspinatus, infraspinatus, and teres minor muscles all attach to the GT, and the combined effects of their forces are pivotal in maintaining proper shoulder function. Given the nature of these insertions, the direction of displacement can be anticipated. Most GT fractures involved the supraspinatus and infraspinatus facets, leading to superior and posterior GT displacement. The posterior displacement is difficult to measure because it is often underestimated and can lead to clinical impingement [2].
In the case of a comminuted fracture of the greater tubercle (GT), it is possible to observe two distinct fragments displaced in different directions. One fragment may be displaced in a superomedial direction, connected to the supraspinatus tendon, while another fragment may be displaced in a posteromedial direction, linked to the infraspinatus tendon [3].
The greater and lesser tuberosities receive small perforators from the anterior and posterior circumflex arteries. In addition, circumflex arteries and the nearby thoracoacromial, supra, and subscapular arteries are also anastomosed numerous times extraosseously. This vascular network explains why isolated fractures of the tuberosity rarely result in osteonecrosis of the humeral head [2, 9].
Most fractures of the greater tuberosity of the humerus can be satisfactorily treated non-surgically [10]. It should be noted that conservative treatment does not imply abandoning the lesion but will require close and serial follow-up with a rehabilitation program that restores function and mobility. Displaced fractures have been treated with various surgical methods, including open or percutaneous reduction and internal fixation (ORIF) and arthroscopically assisted fixation. The choice of fixation and approach is influenced by the patient’s specific circumstances and the fracture’s type, morphology, and characteristics [2].
Standard radiographs are typically used to diagnose these injuries, which usually present as acute shoulder pain with a decreased range of motion. In most cases, computed tomography (CT) is recommended because the evaluation of a 3D structure as the greater tuberosity and its position is not easily determined with simple X-rays. Mainly, it is advantageous when the fracture pattern cannot be adequately defined, and displacement and morphology fracture fragment morphology remain unclear [2, 3]. That can affect the surgical approach, technique, and selection of the implant. CT scans are also helpful for obese patients. That’s why CT scans with coronal and sagittal plane reconstructions are being obtained in the emergency room setting with increasing frequency. However, a good quality complete shoulder radiographic series should preclude obtaining a CT scan in most cases.
Ultrasonography and even magnetic resonance imaging may be helpful, especially in fractures associated with instability.
Most authors agreed that surgical treatment of isolated GT fractures is indicated in patients with a displacement of 5 mm or more. Still, there is a trend to be more aggressive in this limit. Some authors suggest that patients with as little as 3 mm of superior displacement may benefit from surgical reduction and fixation in active [10]. Patients with posterior-superior GT displacement had significantly worse outcomes than those with anterior-inferior or anterior-superior GT displacement. It is unclear, though, how much posterior GT displacement is “acceptable” [3].
With a longer life expectancy and increased physical activity in all age groups, isolated tuberosity fractures of the proximal humeral are expected to rise [2]. For this reason, orthopedic surgeons who treat shoulder trauma must manage different techniques to treat displaced greater tuberosity fractures to be applied in the indicated situation to optimize outcomes.
2. Evaluation
The greater tuberosity is a significant anatomical structure, and shoulder external rotation and abduction depend on its integrity. Greater tuberosity isolated fractures are frequently undetectable on initial radiographs because they are so subtle [11].
These patients arrive holding the injured extremity close to the axial skeleton. Ecchymosis may extend into the axilla and distally along the upper arm, and there is swelling around the upper shoulder, according to an examination. In the acute setting, it is challenging to distinguish tuberosity fracture from cuff pathology clinically; imaging tests are essential to make this critical distinction. Patients will not tolerate the cuff strength test against resistance in both scenarios. A complete neurovascular examination should be performed as nerve injuries occur in one-third of greater tuberosity fracture-dislocations, with full recovery in most cases after several months. In addition, there may also be accompanying glenohumeral dislocations, which must be reduced promptly.
Neurovascular assessment is mandatory. We should complete a global evaluation of the brachial plexus, but it is essential to address with care four nerves: the axillary, musculocutaneous, radial, and suprascapular nerves. The axillary nerve, originating from the posterior cord of the brachial plexus, innervates the deltoid and teres minor muscles. A meticulous assessment of the axillary nerve involves evaluating the range of motion of the shoulder joint and testing the strength of deltoid muscle contraction. Clinical examination techniques, such as the “empty can” test, aid in detecting potential axillary nerve injuries or impingements, often resulting from trauma or overuse. The musculocutaneous nerve, emerging from the lateral cord of the brachial plexus, innervates the biceps, brachial, and brachialis muscles and provides sensory innervation to the lateral forearm. During the examination, the motor function of the biceps brachii is assessed through resistance testing and evaluating the elbow flexion strength. Sensory assessment involves evaluating the sensory perception on the lateral forearm to detect any areas of hypoesthesia or altered sensation. Greater tuberosity fractures are frequently associated with glenohumeral dislocation; in these cases, the radial nerve is the second nerve affected in shoulder dislocations (12.8%) after the axillary nerve [12]. Functional implications are debilitating, including wrist and finger drops. Most palsies recur without treatment in 3 to 6 months, so recovery rates are high. An EMG should be done if there is not any improvement in function after 3 to 6 months. The suprascapular nerve, originating from the upper trunk of the brachial plexus, innervates the supraspinatus and infraspinatus muscles, contributing to shoulder movement and stability. Examination techniques may involve evaluating the strength of these muscles through resisted movements and assessing any potential muscle atrophy. Acute assessment is complicated due to the fracture, but continuous evaluation during follow-up is necessary. Advanced diagnostic tools, including electromyography (EMG) and nerve conduction studies, can provide valuable insights into these nerves’ functionality and potential dysfunctions.
Additionally, imaging modalities such as magnetic resonance imaging (MRI) and ultrasound can assist in visualizing the nerves and surrounding structures, aiding in diagnosing nerve compressions, injuries, or pathologies. An urgent angiogram evaluation is necessary to determine whether vascular intervention is required in the presence of an expanding hematoma, the absence of proximal pulses, and the emergence of upper extremity neuropathy. Even so, vascular injuries in this type of fracture are uncommon.
Isolated fracture of the tuberosity may lead to concomitant rotator cuff tears, which may be the etiology of the patient’s persistent discomfort after fracture union.
The initial technique to detect a fracture of the greater tuberosity of the humerus is plain x-rays. It is recommended to perform an AP view in external rotation and an AP view with a caudal inclination of 15° to define greater tuberosity displacement most accurately. In most situations, displacement is underestimated.
If the x-ray shows us an evident displacement of >5 mm, surgery can be considered based on the activity expectations of each patient. On images, where the degree of displacement is not evident or is borderline (3 to 5 mm), other diagnostic tests may be used, and CT is our gold standard.
If a fracture is suspected, but not identified on radiographs or with a borderline displacement, computed tomography (CT) or MRI may be obtained. MRI has the advantage of evaluating the rotator cuff, bone edema, and labral injuries. In some situations, ultrasound is being chosen as the evaluation modality in many centers when initial radiographs do not provide clear information because more experience is being gained by an increasing number of professionals and it is a non-invasive technique (PoCUS – Point of Care Ultrasound) [2, 11, 13].
The greater tuberosity is an important anatomic structure and its integrity is important for shoulder abduction and external rotation. Isolated fractures of the greater tuberosity are often subtle and may not be detected initially.
3. Surgical treatment
The goal of surgical treatment is to restore anatomy and allow early movement with stable fixation. The selection of an appropriate surgical technique and implant depends on the size of the fragment, the amount of displacement, the level of comminution, and the presence of osteoporosis.
Positioning of the patient is critical to improve visualization of the fragments and adequate implant placement for fixation, and most authors recommend the beach chair position (Figure 1) for both arthroscopic, open or percutaneous techniques, because it allows manipulation of the arm during the procedure, and it is easy to orient. Surgery may also be performed with minimal assistance with the aid of mechanical arm fixation devices such as assist arm. Although the position with which the surgeon is most comfortable and has more experience should be used, being the position in lateral decubitus with longitudinal traction of the affected extremity also valid (Figure 2).

Figure 1.
Chair position.
Figure 2.
Lateral decubitus with longitudinal traction.
The anesthesia used is a combination of general anesthesia and regional block for intraoperative pain control. If we selected arthroscopically assisted techniques, it is mandatory to optimize patient’s blood pressure to minimize bleeding and facilitate visualization. The local use of adrenaline with a local anesthetic minimizes pain and facilitates the anesthesiologist blood pressure control.
3.1 Open reduction
Classically, open reduction and internal fixation have been selected for displaced greater tuberosity fractures. Theoretically, it allows a better visualization and facilitates reduction of the fragment with acceptable rates of union and low rates of complications, with good postoperative outcomes. We can choose between two approaches for this fixation, the deltopectoral approach, which is usually selected in those situations where we need to use a plate, and the transdeltoid approach which may be applied with a longitudinal incision or through a standard anterolateral approach [14, 15].
Several fixation techniques have been described to achieve reduction and stabilization, including trans osseous sutures, locking plates with or without suture augmentation, and screw fixation via open or closed reduction. Each of these techniques is briefly described below.
Trans osseous sutures with non-absorbable sutures passing through the rotator cuff tendon are an option that has shown good effects in biomechanical studies compared to suture anchor techniques in the treatment of greater tuberosity fractures [16], being preferable in patients with poor bone quality. Trans osseous suture allows the fragment fixation obviating the need for a second surgery for implant removal [17].
Open reduction and internal fixation with locking plates combined or not with suture reinforcement are described as a very useful technique for the treatment of greater tuberosity fractures, especially in osteoporotic bone with big fragments [18, 19]. Open plate osteosynthesis provides accurate reduction under direct visualization, rigid fixation of the avulsed fragment, and early mobilization facilitating good functional outcomes, decreasing the possibility of reduction loosening and secondary displacement [20]. The preferred approach for plate fixation is the deltopectoral approach but recent studies have shown promising results with shorter plates that need smaller incisions for placement [14, 20]. This lower profile plates, not specific for this greater tuberosity fractures, have been described to avoid or reduce the complication associated with classic plates and maintaining the rates of union and functional recovery [20]. For these techniques, the use of an anterolateral approach has demonstrated non-inferior outcomes with less complications [21].
Al last, percutaneous fixation with cannulated screws with or without washers has the advantages of a minimally invasive technique, less intraoperative blood loss, shorter hospital stays, and fewer complications related to the incision [22, 23]. Despite this, a non-despicable rate of postoperative stiffness is reported in patients treated with this method [24]. The handicap to performing this minimally invasive technique is confirming anatomical reduction. It is not easy to achieve GT anatomical restoration by closed maneuvers, and in the case of using high compression techniques such as screws with a washer, we may generate a malposition due to overreduction by compression. Comminuted fractures and osteoporotic bones may make percutaneous screw fixation difficult, increasing the hazard of malreduction. In these cases, using devices such as percutaneous low-profile plates or classical plates through an open approach may be preferable [20].
3.2 Arthroscopic repair techniques
Arthroscopically assisted fixation has gained popularity because it brings the “best of both worlds”. When we have a small or osteoporotic fragment, with comminution, we may reduce it under direct visualization in a way like the open technique and we can complete a less invasive fixation with a percutaneous technique. Arthroscopically techniques for rotator cuff tears increase the rigidity of the fixation and favor tension distribution to bone also in osteoporotic bone.
Multiple techniques have been described, but the most widespread and accepted by the authors is perhaps the arthroscopic double-row suture anchor fixation technique (ADSF).
With the patient under general anesthesia, the patient is positioned in the beach chair position. Next, a posterior portal is formed with 2 cm inferior and 2 cm medial to the posterolateral corner of the acromion [22]. An arthroscope is inserted through the posterior portal, and we perform a complete intraarticular examination as a diagnostic arthroscopy after irrigation of the hemarthroses caused by the fracture. Next, we create an anterior working portal through the rotator interval and treat any concurrent pathology found during the arthroscopic examination. The arthroscope is then advanced through the posterior portal to the subacromial space, and a working portal is established 2 cm lateral to the acromion’s anterolateral corner [25, 26, 27, 28]. All subacromial pathology is addressed currently.
We identify the fracture and with the help of a shaver and a burr, debridement is performed under the fracture bed at the humerus. This step also serves to create a bleeding bone surface conducive to healing. With the aid of an arthroscopic grasper and a probe, we reduce the fracture to its anatomical position. Then, correct fracture reduction is confirmed with fluoroscopy.
Next, a knotless self-reinforcing double-row repair is performed with four anchors (two medial anchors and two lateral anchors). In very large fragments, it may be necessary to add more anchors.
Through the anterolateral working portal, two medial anchors (one anteromedial and one posteromedial) loaded with suture tape are inserted into the articular margin of the humeral head, medial to the fracture bed. Maintaining a 15 mm gap between each medial anchor in the anteroposterior direction is recommended. The medial sutures are passed through the intact rotator cuff.
An arthroscopic forceps and suture passer are used to insert each end of the suture tape through the rotator cuff tendon and 3 to 5 mm medial to the bone fragment.
Next, we proceed to implant the lateral row of suture anchors that are placed similar to the medial anchors. The two anchors inserted lateral to the fracture bed are loaded with one limb of the suture tapes from each of the medial anchors, and the repair is completed by tying the sutures above the fracture fragment (Figure 3).
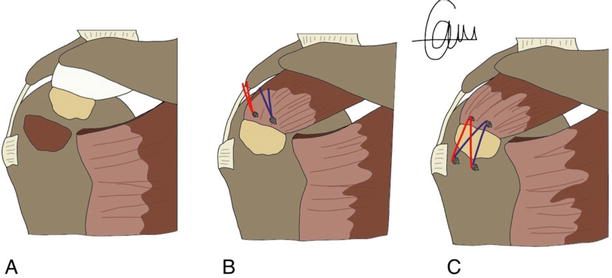
Figure 3.
Illustration of the arthroscopic reduction and double-row suture anchor fixation technique. A. GT fracture B. The 2 suture anchors are placed medial to the fracture bed, and the sutures are then threaded through the intact rotator cuff. C. Each of the two knotless anchors is loaded with a suture limb from each of the medial anchors before being inserted lateral to the fracture bed. The sutures are then tied above the fracture fragment to complete the repair.
Under both direct arthroscopic visualization and fluoroscopy, the correct stability and reduction are confirmed in the passive range of motion of the shoulder. It is important to use both views as relying on arthroscopic viewing without fluoroscopic viewing can lead to poor reduction.
We should remember that any concomitant pathology identified arthroscopically must be noted and repaired after fixing the fracture.
It is worth mentioning another arthroscopic technique widespread among the authors, which is the suture bridge technique with reported very good results and excellent satisfaction in practically all patients (Figure 4) [29, 30, 31].
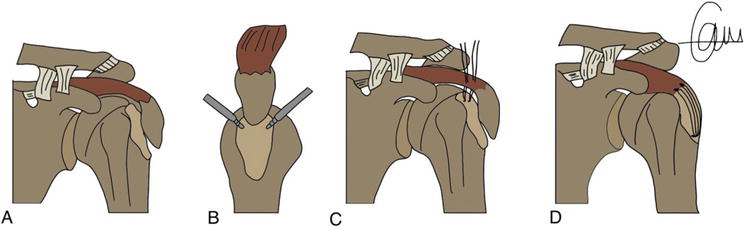
Figure 4.
Illustration of the arthroscopic suture bridge fixation technique. A. GT fracture; B. insert two metal anchors at the articular margin of the humeral head through the intact cuff attached to the GT fragments; C. A nylon is passed through a needle and then the four limbs of 1 double-loaded anchor are retrieved through the intact sleeve; D. Sutures are tensioned and secured over the fracture.
Portals of entry, debridement of the fracture bed, and subsequent steps are common to the above-mentioned technique. The difference is that, here, we use different combinations of sutures. In this technique, we first insert two metal anchors at the articular margin of the humeral head through the intact cuff attached to the GT fragments [30]. A nylon is passed through a needle and then the four limbs of 1 double-loaded anchor are retrieved through the intact sleeve. The medial row sutures stitched over the fracture help to reduce it. With knotless anchors positioned in the vertical part of the tuberosity, distal to the fracture, sutures were tensioned and laterally secured. The lateral row anchors are inserted into the cortical bone of the proximal humerus. Due to the hardness of the cortical bone, it is recommended to pre-drill with the drill beat and then insert the lateral row anchors [29].
Another technique, the authors prefer, is the arthroscopic reduction and trans osseous augmented suture fixation technique useful in osteoporotic patients [32, 33]. A trans osseous tunnel is made, establishing the lateral entry point 2 cm below the lateral fracture margin to prevent cracking of the cortex. A lateral cortical augmentation can be used to avoid any peak stress on sound bone below the fracture margin [33]. An implant is then anchored with three different loaded sutures in the front eyelet of this implant. The sutures, exiting the trans osseous exit point toward the crater fracture, are passed posteriorly to the tendon of the avulsed fragment. Sutures are closed in a mattress fashion over the fragment reducing the fracture.
A parachute suture technique has been proposed for complicated fracture patterns, such as split, comminuted, or multi-fragmentary fracture patterns frequently treated with open reduction and internal fixation [34]. In this parachute arthroscopic procedure, four inverted horizontal knotless mattress sutures are combined with two reinforcing knotted mattress sutures for fracture fixation [35].
Among the different arthroscopic reduction alternatives, no clinical evidence exists that one is superior to the other. What has been shown is that suture anchor constructions may be superior in osteoporotic or multi-fragment fractures where plates or screws may further damage the fragments [28, 36].
3.3 Postoperative follow-up
Postoperative tuberosity fractures follow a protocol like the post-rotator cuff repair patient. Also, minimally displaced fractures of the greater tuberosity of the humerus can be associated with a rotator cuff tear, in this case, the prognosis is worse, and rehabilitation will have to be more focused on performing exercises to restore shoulder cinematics, with special focus in rotator cuff muscles [37].
In the immediate postoperative period of arthroscopic repair, the patient remains in an abduction sling to relieve tension on the supraspinatus tendon and greater tuberosity, one may support the arm in abduction, so the patient is placed in a sling with abduction. This can be done with an airplane splint or a shoulder abduction cushion. We need to focus on passive exercises while maintaining elbow and hand motion [36]. These passive exercises are initiated from the second postoperative day. Passive forward flexion and abduction are allowed and progressed gradually after 1 week preferably under physiotherapist supervision [36]. Formal physical therapy for active-assisted motion begins at 4 weeks, while strengthening exercises are initiated when radiographs showed apparent evidence of fracture healing, which commonly occurs 2–3 months after surgery.
Radiographs are regularly checked in the postoperative period to monitor fracture reduction and document healing [36]. At 6 weeks, active ROM exercises of the shoulder are usually performed and tolerated without pain.
After open reduction, patients are placed in a standard shoulder sling in the immediate postoperative period. The sling is worn for 4–6 weeks. Active motion of the elbow, wrist, and hand, as well as gentle passive exercises, are instituted since day one [20]. At 2 weeks, patients start formal, standardized physical therapy, including passive Range-of-motion (ROM) exercises for elevation and external rotation. At 6 weeks, they begin internal rotation stretching and active-assisted motion. Cuff strengthening begins gently, as motion and pain allowed, after 10–12 weeks. Formal physical therapy continues until full or maximal improvement in motion and strength has been achieved [18]. In general, the authors who applied open surgery started the exercises later than the groups that treat with arthroscopy.
However, some studies, such as that of Liao et al. [38], who compared open vs. arthroscopic surgery, described a similar rehabilitation protocol in the group treated with ORIF and the group treated with arthroscopy.
What is clear is that the literature tells us that the sooner rehabilitation is started in a safe and consensual manner, the better the results are in terms of mobility, stiffness, and residual pain. Even after significant reconstruction, early passive movement in accordance with pain tolerance can typically be started after the first postoperative day. The patient’s capacity, expectations, and the strength and stability of the repair all need to be considered when designing the rehabilitation program.
3.4 Difference in outcomes between open and arthroscopic reduction
Huntley et al. [1] completed a systematic review that showed that patients treated arthroscopically reported slightly superior outcomes compared to patients receiving open reduction internal fixation. The open group had better postoperative forward flexion and external rotation, but the arthroscopic group had better abduction. But noted that most patients were satisfied with outcomes regardless of the technique used.
The extensive dissection required to expose the fracture fragments in open surgery can cause postoperative stiffness, and locking plates have been associated with a higher rate of subacromial impingement [38]. Irritation and protrusion of the hardware were frequently reported in the group treated with open surgery, which required reoperation; the arthroscopic reduction significantly reduced that complication [27]. As arthroscopic techniques improve, the indications for arthroscopic treatment of articular fractures expand. The main benefit of arthroscopic fixation of greater tuberosity fractures is that concurrent injuries, like labral and rotator cuff tears, can be identified and treated simultaneously [38].
The level of expertise required may constrain the use of arthroscopic repair in treating displaced greater tuberosity fractures. A properly executed open technique is preferable to a poorly executed arthroscopic procedure. Therefore, despite being an economically more expensive and technically demanding technique with a longer learning curve, arthroscopic reconstruction offers several advantages over open surgery that should not be ignored.
4. Non-surgical treatment
As we have mentioned, most authors recommend surgical treatment in active patients with a displacement greater than 5 mm and in athletes and workers involving force movements above the shoulder if the displacement is greater than 3 mm. In the literature, there are few examples of functional results in non-operatively treated patients with minimal displacement. Platzer et al. [10] studied displacements of the greater tuberosity of the humerus and the influence on the functionality of the humerus after recovery. Patients with a displacement between 1 and 3 mm and no displaced fractures had equal results. However, patients who had a displacement of more than 3 mm had worse outcomes than those with a smaller displacement, though this was statistically insignificant. Patients with a displacement of more than 5 mm did statistically worse. This supports the recommendation of surgical stabilization in athletes or heavy laborers with a displacement of more than 3 mm, and it should be considered in every active patient.
The period of immobilization varies from 1 to 4 weeks in studies [10, 39, 40, 41, 42]. We discovered no significant differences in outcome even though Mitella slings were frequently used on younger patients and Gilchrist bandages were preferred for elderly patients to achieve immobilization [40]. After this period of immobilization, physiotherapy and rehabilitation programs with strengthening and mobility exercises are necessary.
Women and younger patients had significantly better results with non-operative treatments. Men showed a significant trend in secondary displacements [10].
Postoperative tuberosity fractures follow a protocol similar to the post-rotator cuff repair patient. Also, minimally displaced fractures of the greater tuberosity of the humerus can be associated with a rotator cuff tear; in this case, the prognosis is worse, and rehabilitation will have to be more focused on performing exercises to restore shoulder cinematics, with particular focus in rotator cuff muscles [37].
The patient is kept in an abduction sling for the first few days following surgery, focusing on passive exercises while maintaining elbow and hand motion [36]. On the second postoperative day, these pendulum exercises are begun. After a week, passive abduction and forward flexion are permitted and progress gradually [38]. Formal physical therapy for active-assisted motion starts at fourth week while strengthening exercises are initiated when radiographs show apparent evidence of fracture healing, commonly occurring 3 months after surgery.
Radiographs are regularly checked in the postoperative period to monitor fracture reduction and document healing [36]. At 6 weeks, active ROM exercises of the shoulder are usually performed and tolerated without pain.
5. Complications
A review was conducted in PubMed, Embase, and Scopus databases to identify relevant studies reporting complication rates in surgically managed greater tuberosity fractures [2, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52]. Outcomes were variable between series, with heterogeneous reports and data, and limited studies with high level of evidence were obtained. Complications were categorized into surgical site infection, nerve injury, implant-related issues, restricted range of motion, and other adverse events. The pooled complication rates for open and arthroscopic approaches were calculated based on each study’s reported cases and total number of patients.
5.1 Open surgery complications
The pooled complication rate for open surgery was 17.2% (12.7–22.9%). Surgical site infections were the most common complication in 8.1% (4.7–13.9%) of cases. Nerve injuries were identified in 9.5% (5.8–15.4%) of patients. Implant-related complications were reported in 4.3% (2.1–8.5%) cases. Restricted range of motion and other complications collectively constituted 2.1% (0.9–4.9%) and 2.3% (1.0–5.3%) of cases, respectively.
5.2 Arthroscopic surgery complications
The pooled complication rate for arthroscopic surgery was 12.8% (8.3–19.5%). Notably, no surgical site infections were reported in the arthroscopic group. Nerve injuries were observed in 6.7% (4.0–11.1%) of patients. Implant-related complications occurred in 5.1% (2.7–9.5%) of cases. Restricted range of motion and other complications collectively constituted 1.9% (0.7–4.9%) and 1.7% (0.6–4.7%) of cases, respectively.
Based on the surgical approach, surgically treated greater tuberosity fractures exhibit varying complication rates. Arthroscopic techniques generally demonstrate lower overall complication rates, highlighting potential advantages such as reduced surgical site infections and comparable nerve injury rates.
Even we have found series with limited descriptions of shoulder stiffness, these complications have been described as the most frequent in proximal humeral surgery with rates as elevated as 25. To prevent it, formal physiotherapy is carried out with early and progressive passive range of motion and stretching [2]. The risks inherent to arthroscopic surgery must be considered, such as fluid extravasation, iatrogenic rotator cuff injury, cartilage injury, or neurovascular injury, especially the axillary nerve injury [27].
The neurological injuries frequently associated with fractures of the greater tuberosity of the humerus consist of injuries to the brachial plexus and the axillary nerve. In situations where there is a shoulder muscle weakness that is persistent, electromyography is very interesting. Less frequently occurring were vascular lesions (axillary artery and vein) [40].
6. Conclusion
Arthroscopic reduction and fixation of displaced GT fractures is a safe, effective, and minimally invasive procedure for optimal fracture healing and patient satisfaction and a reliable alternative to open fixation for fractures of the GT of the humerus.
We must emphasize the importance of having good preoperative images to not overlook concomitant injuries or secondary fracture patterns.
The arthroscopic technique has innumerable advantages, such as minimally invasive technique, allows you to visualize and addresses concomitant intraarticular pathology, some authors describe faster recovery [25], and no removal of implanted material when using the different suture systems. Other benefits of arthroscopic surgery include its minimally invasive nature, which results in less blood loss and soft tissue disruption, the ability to examine and treat other injured shoulder structures, reduced radiation exposure for both patient and doctor and improved biomechanical strength with suture anchor constructs [36].
On the other hand, the disadvantages of these techniques are that they are very technically challenging with an early learning curve, a longer operative time than open procedures, and visibility can be problematic in cases with significant bleeding. For this reason, they should be performed by expert shoulder surgeons with enough experience in arthroscopic procedures.
In most cases, greater tuberosity fractures can be successfully treated without surgery. However, patients with >5 mm superior GT displacement have better surgical treatment outcomes. Multiple surgical methods have been described for treating GT fractures and should be carefully and strategically employed according to comminution, displacement, type of patient, and morphology.
References
- 1.
Samuel R, Huntley A, Eva J, Lehtonen A, Joseph Xavier Robin A, Alexandra M, et al. Outcomes of surgical fixation of greater tuberosity fractures: A systematic review. Orthopaedics & Traumatology: Surgery & Research. 2020; 106 (6):1119-1126. DOI: 10.1016/j.otsr.2020.05.005 - 2.
Gruson KI, Ruchelsman DE, Tejwani NC. Isolated tuberosity fractures of the proximal humeral: Current concepts. Injury. 2008; 39 (3):284-298. DOI: 10.1016/j.injury.2007.09.022 - 3.
Rouleau DM, Mutch J, Laflamme GY. Surgical treatment of displaced greater tuberosity fractures of the humerus. The Journal of the American Academy of Orthopaedic Surgeons. 2016; 24 (1):46-56. DOI: 10.5435/JAAOS-D-14-00289 - 4.
Warner JJ, Costouros JG, Gerber C. Fractures of the proximal humerus. In: Bucholz RW, Heckman JD, Court-Brown C, editors. Rockwood & Green’s Fractures in Adults. Ed. 6 ed. Philadelphia, PA: Lippincott William and Wilkins; 2006. pp. 1161-1209 - 5.
Le Minor JM, Tomasi JP, Segonds C, Duparc F. Arterial supply of the proximal humerus and its potential surgical applications. Surgical and Radiologic Anatomy. 2018; 40 (7):831-839 - 6.
Iacobellis C, Piccinini G, Sammartino A, Savarese E, Bisaccia M. Vascular anatomy of the greater and lesser tuberosities of the humerus: An angiographic study. Surgical and Radiologic Anatomy. 2019; 41 (6):663-667 - 7.
Basat HC, Aydin NK, Kizkapan TB, Yazicioglu O. Vascular anatomy of the humeral tuberosities and its relation to anatomical neck fractures: A cadaveric study. Journal of Orthopaedic Surgery and Research. 2017; 12 (1):40 - 8.
Standring S, Borley NR, Collins P, editors. Gray’s Anatomy E-Book: The Anatomical Basis of Clinical Practice. Elsevier Health Sciences; 2016 - 9.
Hertel R, Hempfing A, Stiehler M, Leunig M. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. Journal of Shoulder and Elbow Surgery. 2004; 13 (4):427-433. DOI: 10.1016/j.jse.2004.01.034 - 10.
Platzer P, Kutscha-Lissberg F, Lehr S, Vecsei V, Gaebler C. The influence of displacement on shoulder function in patients with minimally displaced fractures of the greater tuberosity. Injury. 2005; 36 (10):1185-1189 - 11.
White EA, Skalski MR, Patel DB, et al. Isolated greater tuberosity fractures of the proximal humerus: Anatomy, injury patterns, multimodality imaging, and approach to management. Emergency Radiology. 2018; 25 :235-246. DOI: 10.1007/s10140-018-1589-8 - 12.
Lorente A, Mariscal G, Barrios C, Lorente R. Nerve injuries after glenohumeral dislocation, a systematic review of incidence and risk factors. Journal of Clinical Medicine. 2023; 12 :4546. DOI: 10.3390/jcm12134546 - 13.
Patten RM, Mack LA, Wang KY, Lingel J. Nondisplaced fractures of the greater tuberosity of the humerus: Sonographic detection. Radiology. 1992; 182 :201-204 - 14.
Xue G, Chahal K, Lim T, Hu S, Li S, Liu J. Titanium mini locking plate with trans-osseous sutures for the treatment of humeral greater tuberosity fracture osteosynthesis versus philos: A retrospective view. International Orthopaedics. 2018; 42 (10):2467-2473 - 15.
Gavaskar AS, Chowdary N, Abraham S. Complex proximal humerus fractures treated with locked plating utilizing an extended deltoid split approach with a shoulder strap incision. Journal of Orthopaedic Trauma. 2013; 27 (2):73-76. DOI: 10.1097/BOT.0b013e31825cf545 - 16.
Ju J, Ma M, Ding Z, Zhang Y. Clinical article. A transosseous suture as an alternative to suture anchor on anterior-avulsion greater tuberosity fragment fixation in neer three-part proximal humeral fracture: A biomechanical study. Orthopaedic Surgery. 2022; 15 (8):2132-2137 - 17.
Cheng MF, Hung SH, Su YP, Chiang CC, Chang MC, Chiu FY. Displaced isolated greater tuberosity fractures of elder adults treated with plate osteosynthesis. Journal of the Chinese Medical Association. 2019; 82 (4):318-321. DOI: 10.1097/JCMA.0000000000000049 - 18.
Gillespie RJ, Johnston PS, Gordon VA, Ward PJ, Getz CL. Using plate osteosynthesis to treat isolated greater tuberosity fractures. American Journal of Orthopedics (Belle Mead, N.J.). 2015; 44 (8):E248-E251 - 19.
Lee W, Shin H, Kim K. Open reduction and stable internal fixation using a 3.5-mm locking hook plate for isolated fractures of the greater tuberosity of the humerus: A 2-year follow-up study using an innovative fixation method. Clinics in Orthopedic Surgery. 2021; 13 :293-300 - 20.
Zeng LQ , Chen YF, Jiang YW, Zeng LL, Miao XG, Liang WG. A new low-profile anatomic locking plate for fixation of comminuted, displaced greater tuberosity fractures of the proximal humerus. Journal of Shoulder and Elbow Surgery. 2021; 30 (6):1402-1409. DOI: 10.1016/j.jse.2020.08.036 [Epub 2020 Sep 16] - 21.
Xie L, Zhang Y, Chen C, Zheng W, Chen H, Cai L. Deltoid-split approach versus deltopectoral approach for proximal humerus fractures: A systematic review and meta-analysis. Orthopaedics & Traumatology, Surgery & Research. 2019; 105 (2):307-316. DOI: 10.1016/j.otsr.2018.12.004 [Epub 2019 Mar 14] - 22.
Wu X, Li F, Ying J, Chen B, Su Y-X, Sun H-Y. Clinical effects between cannulated screw and bone plate internal fixation for humeral tuberosity fracture: A meta analysis. Zhongguo Gu Shang. 2021; 34 :180-190 - 23.
Liehu C, Weizong W, Shaojun S, Haihang L. Comparison of effectiveness between minimally invasive cannulated screw and open reduction and plate fixation in treatment of humeral greater tuberosity fracture. Chinese Journal of Reparative and Reconstructive Surgery. 2013; 27 (4):418-422 - 24.
Yoon T, Choi C, Choi Y. Clinical outcomes of minimally invasive open reduction and internal fixation by screw and washer for displaced greater tuberosity fracture of humerus. Journal of Shoulder and Elbow Surgery. 2017; 27 :1-5 - 25.
Godin JA, Katthagen JC, Fritz EM, Pogorzelski J, Millett PJ. Arthroscopic treatment of greater tuberosity avulsion fractures. Arthroscopy Techniques. 2017; 6 (3):e777-e783. DOI: 10.1016/j.eats.2017.02.006 - 26.
Ji JH, Shafi M, Song IS, Kim YY, McFarland EG, Moon CY. Arthroscopic fixation technique for comminuted, displaced greater tuberosity fracture. Arthroscopy. 2010; 26 (5):600-609. DOI: 10.1016/j.arthro.2009.09.011 [Epub 2010 Feb 26] - 27.
Kokkalis ZT, Papanikos E, Bavelou E, Togias G, Sioutis S, Mavrogenis AF, et al. Arthroscopic reduction and fixation of greater tuberosity fractures of the humerus. European Journal of Orthopaedic Surgery and Traumatology. 2021; 31 (6):1055-1060. DOI: 10.1007/s00590-020-02835-8 [Epub 2021 Jan 2] - 28.
Patel SP, Nuelle CW, Hartzler RU. Arthroscopic reduction and internal fixation of proximal humerus greater tuberosity fracture. Arthroscopy Techniques. 2020; 9 (9):e1363-e1367. DOI: 10.1016/j.eats.2020.05.019 - 29.
Park SE, Ji JH, Shafi M, Jung JJ, Gil HJ, Lee HH. Arthroscopic management of occult greater tuberosity fracture of the shoulder. European Journal of Orthopaedic Surgery and Traumatology. 2014; 24 (4):475-482. DOI: 10.1007/s00590-013-1212-3 [Epub 2013 Apr 5] - 30.
Ji JH, Jeong JJ, Kim YY, Lee SW, Kim DY, Park SE. Clinical and radiologic outcomes of arthroscopic suture bridge repair for the greater tuberosity fractures of the proximal humerus. Archives of Orthopaedic and Trauma Surgery. 2017; 137 (1):9-17. DOI: 10.1007/s00402-016-2586-6 [Epub 2016 Oct 26] - 31.
Li R, Cai M, Tao K. Arthroscopic reduction and fixation for displaced greater tuberosity fractures using the modified suture-bridge technique. International Orthopaedics. 2017; 41 (6):1257-1263. DOI: 10.1007/s00264-017-3461-y [Epub 2017 Apr 11] - 32.
Fleega BAN, Kareim S. Arthroscopic reduction and transosseous suture fixation of avulsed displaced shoulder greater tuberosity fracture. Arthroscopy Techniques. 2021; 10 (3):e821-e830. DOI: 10.1016/j.eats.2020.10.074 - 33.
Chillemi C, Proietti R, Rengo M, Damo M, Paolicelli D, Castagna A. Fracture avulsion of the greater tuberosity: Arthroscopic transosseous augmented technique. Arthroscopy Techniques. 2021; 10 (5):e1233-e1238. DOI: 10.1016/j.eats.2021.01.017 - 34.
Velasquez Garcia A, Abdo G, Ingala ML. Arthroscopic parachute technique for split-type greater tuberosity fractures. Arthroscopy Techniques. 2023; 12 (3):e349-e355. DOI: 10.1016/j.eats.2022.11.014 - 35.
Stueve J, Fenlin J. The parachute technique: Repair of displaced 2-part proximal humerus fractures. Techniques in Shoulder & Elbow Surgery. 2009; 10 :125-129. DOI: 10.1097/BTE.0b013e3181b3555c - 36.
Andrew H, Larry F. Arthroscopic management of displaced greater tuberosity fractures. Arthroscopy Techniques. 2021; 10 :e1055-e1060. DOI: 10.1016/j.eats.2020.12.006 - 37.
Fjalestad T, Hole MØ, Blücher J, Hovden IA, Stiris MG, Strømsøe K. Rotator cuff tears in proximal humeral fractures: An MRI cohort study in 76 patients. Archives of Orthopaedic and Trauma Surgery. 2010; 130 (5):575-581. DOI: 10.1007/s00402-009-0953-2 [Epub 2009 Aug 14] - 38.
Liao W, Zhang H, Li Z, Li J. Is arthroscopic technique superior to open reduction internal fixation in the treatment of isolated displaced greater tuberosity fractures? Clinical Orthopaedics and Related Research. 2016; 474 (5):1269-1279. DOI: 10.1007/s11999-015-4663-5 [Epub 2016 Jan 4] - 39.
Kumar S, Mishra A, Singh H, Clark D, Espag M, Tambe A. Surgical fixation of isolated greater tuberosity fractures of the humerus-systematic review and meta-analysis. Journal of Clinical Orthopaedics and Trauma. 2021; 23 :101670. DOI: 10.1016/j.jcot.2021.101670 - 40.
Jellad A, Bouaziz MA, Boudokhane S, Aloui I, Ben Salah Z, Abid A. Isolated greater tuberosity fracture: Short-term functional outcome following a specific rehabilitation program. Annals of Physical and Rehabilitation Medicine. 2012; 55 (1):16-24. English, French. Epub 2011 Dec 3. DOI: 10.1016/j.rehab.2011.10.007 - 41.
Mattyasovszky SG, Burkhart KJ, Ahlers C, Proschek D, Dietz SO, Becker I, et al. Isolated fractures of the greater tuberosity of the proximal humerus: A long-term retrospective study of 30 patients. Acta Orthopaedica. 2011; 82 (6):714-720. DOI: 10.3109/17453674.2011.618912 [Epub 2011 Sep 6] - 42.
Rath E, Alkrinawi N, Levy O, Debbi R, Amar E, Atoun E. Minimally displaced fractures of the greater tuberosity: Outcome of non-operative treatment. Journal of Shoulder and Elbow Surgery. 2013; 22 (10):e8-e11. DOI: 10.1016/j.jse.2013.01.033 [Epub 2013 Apr 29] - 43.
Torrens C, Alentorn-Geli E, Mingo F, Gamba C, Santana F. Reverse shoulder arthroplasty for the treatment of acute complex proximal humeral fractures: Influence of greater tuberosity healing on the functional outcomes. Journal of Orthopaedic Surgery (Hong Kong). Jan-Apr 2018; 26 (1):2309499018760132. doi: 10.1177/2309499018760132. PMID: 29486672 - 44.
Verdano MA, Aliani D, Pellegrini A, Baudi P, Pedrazzi G, Cec-carelli F. Isolated fractures of the greater tuberosity in proximal humerus: Does the direction of displacement influence functional outcome? An analysis of displacement in greater tuberosity fractures. Acta Biomedica. 2013; 84 (3):219-228 - 45.
Yin B, Moen TC, Thompson SA, Bigliani LU, Ahmad CS, Levine WN. Operative treatment of isolated greater tuberosity fractures: Retrospective review of clinical and functional outcomes. Orthopedics. 2012; 35 (6):e807-e814 - 46.
Platzer P, Thalhammer G, Oberleitner G, et al. Displaced fractures of the greater tuberosity: A comparison of operative and nonoperative treatment. Journal of Trauma and Acute Care Surgery. 2008; 65 (4):843-848 - 47.
McLaughlin HL. Dislocation of the shoulder with tuberosity fracture. Surgical Clinics of North America. 1963; 43 :1615-1620 - 48.
Dimakopoulos P, Panagopoulos A, Kasimatis G, Syggelos SA, Lambiris E. Anterior traumatic shoulder dislocation associated with displaced greater tuberosity fracture: The necessity of operative treatment. Journal of Orthopaedic Trauma. 2007; 21 (2):104-112 - 49.
Chen CY, Chao EK, Tu YK, Ueng SW, Shih CH. Closed management and percutaneous fixation of unstable proximal humerus fractures. Journal of Trauma and Acute Care Surgery. 1998; 45 (6):1039-1045 - 50.
Ji JH, Shafi M, Song IS, Kim YY, McFarland EG, Moon CY. Arthroscopic fixation technique for comminuted, displaced greater tuberosity fracture. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2010; 26 (5):600-609 - 51.
Bhatia DN, van Rooyen KS, Toit du DF, de Beer JF. Surgical treatment of comminuted, displaced fractures of the greater tuberosity of the proximal humerus: A new technique of double-row suture-anchor fixation and long-term results. Injury. 2006; 37 (10):946-952 - 52.
Rojas JT, Rashid MS, Zumstein MA. How to treat stiffness after proximal humeral fractures? EFORT Open Reviews. 1 Aug 2023; 8 (8):651-661. doi: 10.1530/EOR-22-0118. PMID: 37526247; PMCID: PMC10441249