Comparison of all the article from the literature for the liparthroplasty of trapeziometacarpal joint.
Abstract
Autologous fat injection into osteoarthritic joints (liparthroplasty) has shown high potential in reducing pain and delaying the need for surgical intervention. The liparthroplasty is an alternative and minimally invasive treatment approach for finger and thumb carpometacarpal joint osteoarthritis with only a few studies available. A systematic literature review was performed with a search strategy in MEDLINE databases Google Scholar and Cochrane Library using the following keywords: “autologous fat grafting injection”, “adipose-derived stem cells”, “finger osteoarthritis”, “basal thumb ostheoarthritis”, “lipofilling”. The database was analyzed from inception to August 1st, 2023. About 148 studies were identified; 17 additional articles were found through previous publications (total 165 articles). A total of 150 records resulted after duplicates were removed. Fourteen studies were selected and only 10 respected the inclusions criteria. In all these studies, intra-articular injection of autologous fat into osteoarthritic finger joints and trapeziometacarpal joint reduced pain and improved hand function. The liparthroplasty of osteoarthritic finger joints seems to be a minimally invasive, secure, and valid substitute for traditional surgical interventions. While the outcomes are promising, the lack of a standardized technique to fat processing and the absence of randomized controlled trials impede a thorough assessment of the procedure’s effectiveness.
Keywords
- autologous fat grafting
- adipose-derived stem cells
- basal thumb osteoarthritis
- rhizoarthrosis
- finger osteoarthritis
- regenerative medicine
- joint lipofilling
- liparthroplasty
1. Introduction
Trapeziometacarpal (TM) and finger joint osteoarthritis are a progressive and disabling pathology of the hand [1]. Treatment can be conservative with orthosis, occupational therapy, anti-inflammatory drugs and intra-articular injections with cortisone and hyaluronic acid, resulting in only temporary success [1]. Furthermore, the time- and dose-dependent detrimental effects of the corticosteroids on articular cartilage
2. Materials and methods
The systematic review was delineated following the PRISMA statement [15], using the guidelines described in the Cochrane Handbook for Systematic Reviews of Interventions.
2.1 Data sources and searches
A comprehensive search strategy was defined in collaboration with an independent research librarian and structured to capture all articles relating to autologous fat injection in osteoarthritic finger joints. The search strategy was applied to the MEDLINE databases, Google Scholar and Cochrane Library using the following keywords: “autologous fat grafting injection”, “adipose-derived stem cells”, “finger osteoarthritis”, “basal thumb osteoarthritis”, “lipofilling”. The database was analyzed from inception to August 1st, 2023.
2.2 Inclusion/exclusion criteria
The inclusion and exclusion criteria were defined during the protocol stage. An article was included if the following criteria were fulfilled: the study was a primary study, case report or new technical report; the treatment was an injection of autologous fat with the description of harvesting technique and fat processing technique; follow-up, gender and age of the patients were reported; only studies with a design classification of evidence levels I-V were included.
Data not published on Pubmed, Google Scholar, Cochrane Library literature reviews, letters to editors, book chapters and presentations to congress were also excluded.
2.3 Selection of studies
The titles and abstracts of the studies were independently screened by two authors (MG, SL). The references of all studies and all review articles on the subject were also examined to identify other additional data to be included. This was subsequently followed by the assessment of the full text of the selection of studies. A third reviewer (IT) was helpful for any disagreements that could not be solved by this initial review.
2.4 Data extraction
Two reviewers (MG and SL) analyzed the data on an independent basis. The studies were scored for author name, year of publication, journal, population type and demographics and objective outcome measures.
2.5 Surgical technique
Many different techniques are described. The authors’ preferred technique takes place under local anesthesia at the affected joint (using 5 ml of 1% lidocaine). A tumescent solution is employed for liposuction in the lower abdomen (upper thigh or lateral-gluteal region can also be used as donor site). The tumescent solution is prepared in sterile conditions, with a mixture of 100 ml of sodium chloride solution, 1 ml of 8.4% sodium bicarbonate and 10 ml of 1% lidocaine combined with 5 mcg/ml epinephrine. Roughly 50 ml of this solution is then evenly dispersed within the subcutaneous tissue.
Following a 10-min interval, a 2 mm incision is made in the lower portion of the umbilicus. By using a hemostat forceps, the subcutaneous tissue is dissected, enabling the insertion of a suction cannula (Figure 1). Approximately 15 ml of aspirate is collected and divided into two Luer-lock syringes (Figure 2). A variable amount of 0.5 to 1 ml of adipose tissue is introduced into each joint in a sterile field. To facilitate the insertion of the needle, a slight axial manual traction is applied on the finger, favoring the expansion of the joint space of the interphalangeal, metacarpophalangeal or trapeziometacarpal joint.

Figure 1.
A single umbilical incision was used. The lower abdomen skin was infiltrated with 50 mL solution (600 mg of lidocaine, 1000 mL of saline solution and 1 mL of 1:200,000 adrenaline). The vasoconstrictive effect of adrenalin is clearly visible by hypoperfusion of the skin.
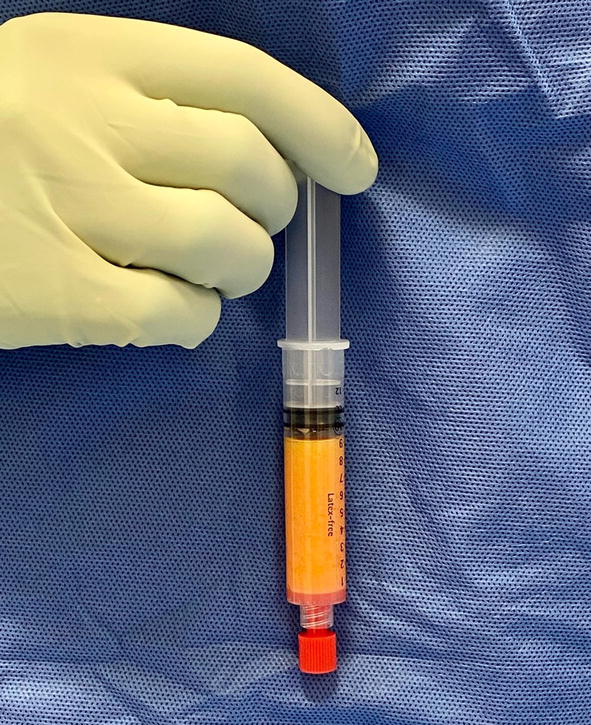
Figure 2.
Decantation and sedimentation allow the product to separate into three layers (aqueous, oil and fat). The oil and aqueous phases are then extracted, while the fat layer is withdrawn for injection.
Depending on the size of each joint treated, fat tissue is injected in the amount that could be injected into the joint without over-pressure. Metacarpophalangeal joints receive a volume of adipose tissue of 1 ml, while the distal interphalangeal joints receive a smaller volume (0.5 ml) (Figures 3 and 4).
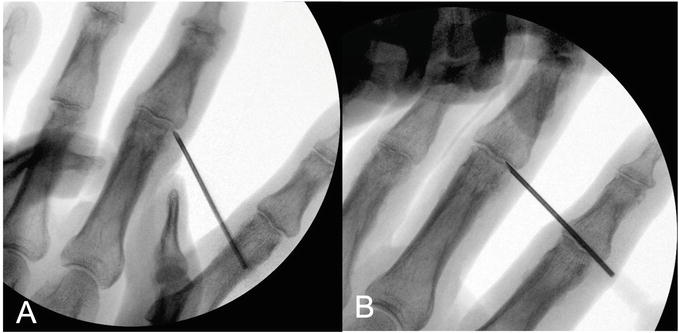
Figure 3.
Liparthroplasty of the proximal interphalangeal joint of the left middle finger in a 60-year-old man. A) Fluoroscopy before the injection. B) with an 18G needle and a 3 mL Luer-lock syringe 0.5 mL of lipoaspirate was injected into the joint. A widening of the joint is clearly visible after the injection.
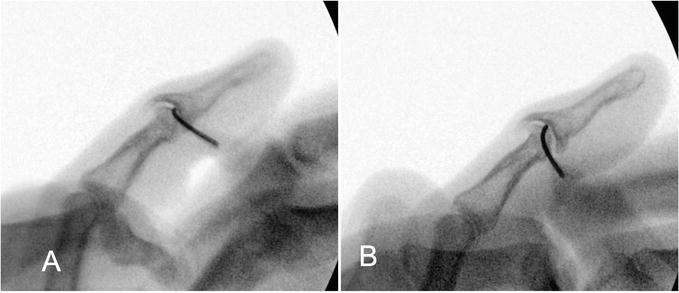
Figure 4.
Autologous fat infiltration of a distal interphalangeal joint of the right ring finger in a 63-year-old man. A) before infiltration. B) Fluoroscopy during injection of 0.5 mL of fat. A widening of the joint is clearly visible after the injection.
The adipose tissue is injected under fluoroscopy guidance. In multiple joint infiltrations, the needle must be changed for each infiltrated joint (Figures 5 and 6).

Figure 5.
Liparthroplasty of the right trapeziometacarpal joint in a 56-year-old woman with a painful Eaton stage I basal thumb osteoarthritis. A) Fluoroscopy before the injection. B) with an 18G needle and a 3 mL Luer-lock syringe 1.5 mL of lipoaspirate was injected into the trapezio-metacarpal joint. C) Fluoroscopy after the procedure without traction.
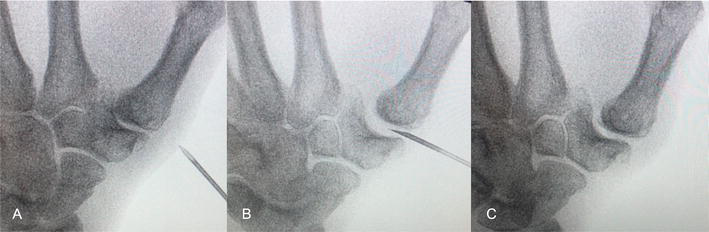
Figure 6.
Autologous fat infiltration of a left trapeziometacarpal joint of a 61-year-old male patient with an Eaton stage II basal thumb osteoarthritis. A) before infiltration. B) Fluoroscopy during injection of 1 mL of fat and C) at the end of the procedure.
Subsequently, a thermoplastic splint is applied for the following 2 weeks. All patients undergo a functional recovery protocol with the occupational therapist.
2.6 Fat processing technique
2.6.1 Centrifugation
Coleman [16] introduced a fat-processing technique for reinjection. This method, still widely used, involves the separation of fat components using high-speed centrifugation. Numerous research studies have documented varying centrifugation configurations [17]. Some of these studies propose that higher levels of centrifugal force could harm the fat cells, resulting in reduced cell viability. Conversely, very low centrifugal forces yield outcomes similar to the simple process of sedimentation [17]. Pulsfort et al. [18] indicated that variations in centrifugation techniques did not lead to significant histological changes in the viability of adipocytes and did not result in apoptotic changes.
2.6.2 Cotton gauze technique
The method of cotton gauze rolling is another commonly utilized approach to isolate harvested fat grafts. In this process, the gathered fat is positioned over the gauze. A forceps or tongue depressor is used to isolate the fat across the gauze. The gauze absorbs fluid and oil, leaving behind the cellular components of the fat graft. As the blood and other elements of lipoaspirate are removed, the harvested fat takes on a more pronounced yellow color. This technique is known to take approximately 2 to 4 minutes, it is cheap with minimal damage to the fat [19].
2.6.3 Decantation
Decantation and sedimentation allow the product to separate into three layers (aqueous, oil and fat). The oil and aqueous phases are then extracted, while the fat layer is withdrawn for injection [20].
2.6.4 Washing and filtration
Lipoaspirate preparation can involve washing and/or filtration, usually conducted within a closed system. These two methods can be carried out individually or in combination. Washing generally involves multiple cycles with lactated Ringer’s solution, while filtration takes place through membranes of various pore sizes [21].
Currently, no single technique exhibits superior results in terms of fat graft take compared to others. Decantation leads to a higher number of viable adipocytes along with undesired cellular components, which ultimately results in lower graft take compared to centrifugation and washing methods [22].
3. Results
A total of 148 studies were identified; 17 additional articles were found through previous publications (a total of 165 articles). A total of 150 records resulted after duplicates were removed. A total of 14 studies were selected and only 10 respected the inclusion criteria (Figure 7).
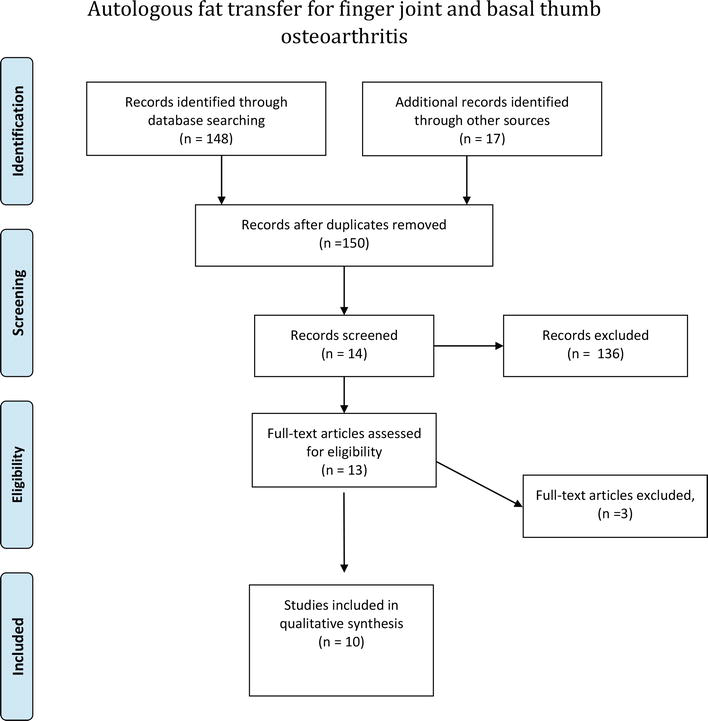
Figure 7.
PRISMA statement of the study
3.1 Study characteristics
Of the 10 included studies, 9 reported on trapeziometacarpal joint injection. Only one was reported on osteoarthritic finger joints. Table 1 summarizes the results.
| Author | Patients | Joint | Eaton classification | Fat grafting technique | Follow up | VAS | Pinch/Grip | DASH/MHQ | Weaknesses |
|---|---|---|---|---|---|---|---|---|---|
| Herold [23] 2014 | 5 patients | TM joint | II -III | Centrifugation (Coleman) | 3 months | Non statistically significant reduction | Non statistically significant improvement | Significant improvement after liparthroplasty | Short follow up, lack of controls, small sample size |
| Bohr [24] 2015 | 1 patient | TM joint | II | Centrifugation (Coleman) | 12 months | N/A | N/A | Significant improvement after liparthroplasty | Lack of clinical parameters, small sample size |
| Herold [25] 2017 | 50 patients | TM joint | II-IV | Centrifugation (Coleman) | 12 months | Significant reduction after liparthroplasty | Significant improvement after liparthroplasty | Significant improvement after liparthroplasty | Lack of clinical parameters, small sample size |
| Haas [26] 2017 | 24 patients, 12 triamcinolone, 12 fat grafting | TM joint | I-III | Mechanical homogenization | 3 months | Significant reduction after liparthroplasty | Non statistically significant improvement | Significant improvement after liparthroplasty | Short follow up, Lack of controls |
| Erne [27] 2018 | 21 patients, 9 fat grafting, 12 resection arthroplasty | TM joint | III-IV | Centrifugation (Coleman) | 12 months | Improvement of VAS but no significant difference | Non statistically significant improvement | Non statistically significant improvement | No randomization, small sample size |
| Haas [28] 2019 | 99 patients | TM joint | I-III | Filtration and mechanical homogenization | 12 months Significant reduction after liparthro-plasty | Non statistically significant improvement | Significant improvement after liparthroplasty | Lack of controls | |
| Forschauer [29] 2020 | 31 patients | TM joint | II-III | Decantation/mech anical homogenzation | 2 years | Significant reduction after liparthroplasty | Non statistically significant improvement | Significant improvement after liparthroplasty | Lack of controls |
| Herold [30] 2022 | 42 patients | TM joint | II -III | Centrifugation (Coleman) | 4 years | Significant reduction after liparthroplasty | Significant improvement after liparthroplasty | Significant improvement after liparthroplasty | Lack of controls |
| Meyer-Marcotty [31] 2022 | 25 patients | MP joint n = 4 PIP joint n = 18 DIP joint n = 3 | N/A | Centrifugation (Coleman) | 44 months (3.7 years) | Significant reduction after liparthroplasty | Significant improvement of Pinch after liparthroplasty | Significant improvement after liparthroplasty | Lack of controls |
| Holzbauer [32] 2022 | 31 patients | TM joint | II-III | Decantation/mech anical homogenzatio | 5.1 years | Significant reduction after liparthroplasty | Significant improvement of Pinch after liparthroplasty | Significant improvement after liparthroplasty | Lack of controls |
Table 1.
The article included in the systematic review was case-control studies (n = 2), case series (n = 7) and a case report (n = 1). The harvested fat processing system was done by centrifugation (n = 6), mechanical homogenization alone (n = 1), mechanical homogenization and filtration (n = 1), decantation and mechanical homogenization (n = 2). None of the above-mentioned studies examined the injected tissue for cell count or viability. Follow-up ranged from 3 months to five years. Only one study analyzed metacarpophalangeal infiltrations of the proximal interphalangeal and distal interphalangeal fingers. In all studies, intra-articular injections of 0.5 mL up to 2 mL of fat into the joints were performed under fluoroscopic guidance.
3.1.1 Indications
The indications where osteoarthritis with radiological findings showing ostearthritis and failed medical treatment.
3.1.2 Pain
In terms of symptomatic pain relief (VAS) after fat grafting, outcomes have been consistently positive. Only one article [23] showed non-statistically significant improvement of the pain.
3.1.3 Strength
Five studies reported non-statistically significant improvement of the strength after the liparthroplasty [23, 26, 27, 28, 29]. In 4 more recent studies [25, 30, 31, 32] with a larger court of patients the authors report statistically significant improvement in strength as well. There is a trend to an improvement of grip and pinch strength after 12 h months (Table 1).
3.1.4 Function of the hand
Statistically significant DASH Score (Disabilities of Arm, Shoulder and Hand) improvement after fat injection is reported in all the studies except one [27].
3.1.5 Complications
No significant complications were reported. One patient who had a hematoma in the donor site and three patients reported hypoesthesia in the skin area supplied by the superficial radial nerve.
3.1.6 Study analysis
Herold et al. [23] conducted a small case series involving five patients with thumb carpometacarpal joint (CMCJ) osteoarthritis (stages II and III). Three months after autologous fat injection, they observed improvements in grip strength, pinch strength and hand function as measured by the DASH score. However, these improvements were not statistically significant compared with preoperative values. The study had limitations, such as short follow-up and a limited sample size. The same authors reported on greater case series with 50 patients and a follow-up of one year, reporting significant reductions in pain, improvements in grip and pinch strength and Quick-DASH scores after intra-articular fat injection.
Bohr et al. [24] reported improvement in DASH scores in a single case of stage II CMCJ arthritis treated with intra-articular fat injection. However, this study is limited by being a single case report without objective clinical evaluation and control groups.
In the first case-control study conducted in 2017 by Haas et al. [26], patients with stage I-III CMCJ arthritis who received autologous fat transplantation or corticosteroid injection were examined. The fat processing technique involved mechanical homogenization, but no details were given about the specific fat product used. After 3 months, the fat group experienced a significant reduction in pain and improvement in quality of life (Quick DASH and Michigan Hand Questionnarire-MHQ scores), while the corticosteroid group, although initially improved, regressed below preoperative levels after six weeks. Grip strength remained unchanged in both groups, and the follow-up period was relatively short.
Erne et al. [27] conducted a case-control study of 21 patients with advanced CMCJ arthritis of the thumb (Eaton stages III and IV). They compared autologous fat grafting with Lundborg resection arthroplasty, with patients given a choice between the less invasive and traditional surgical approaches. The group of patients treated with fat experienced a significantly shorter time to pain resolution (1.7 months compared with 5.7 months in the group of patients treated with resection). Pain levels (Visual Analogue Scale - VAS), grip and pinch strength and DASH scores improved similarly in both groups after 12 months. The duration of the intervention was also significantly shorter in the fat group. However, this study had limitations, such as a small sample size and lack of randomization, which introduced a potential selection bias.
Herold et al. in 2017 reported on a wider group involving 50 patients with one-year-follow-up [25]. In this study, intra-articular lipofilling resulted in a significant reduction in pain, higher values of grip and pinch strength and a lower Quick DASH score.
In 2019 Haas et al. [28] published a study with the largest number of patients, involving 99 patients with symptomatic CMCJ osteoarthritis of the thumb. These patients received 1–2 mL of mechanically homogenized autologous fat. After 12 months, the study demonstrated significant pain reduction and improvements in DASH and MHQ scores. However, grip and pinch strength remained unchanged.
Forschauer et al. [29] in 2020 conducted a two-year follow-up study of 31 patients with stage II and III osteoarthritis. They reported results consistent with other studies, including a significant reduction in pain and improvement in grip and pinch strength following autologous fat injection.
In 2022 Herold et al. reported on a group of 42 patients with a longer follow-up, averaging 4.9 ± 0.7 years [30]. The authors noted that, among the initial 50 consecutive patients, three needed surgical conversion within the first year after the intervention. In comparison to the previously mentioned study [25] they present slightly elevated pain levels during activity (4.0 ± 3.0) and DASH Scores (31 ± 22), although these outcomes remained significantly lower than the pre-intervention levels.
In 2022 Meyer-Marcotty [31] investigated the autologous fat injection of 25 finger joints of the hand with a mean follow-up of 44 months. The median DASH score improved non-significantly from 50 (3 t ± 72) to 25 (0 ± 85). The median level of pain experienced showed a highly significant improvement from 6.0 (1.0 ± 10.0) to 0.5 (0.0 ± 6.5). The median force of pinch grip rose highly significantly from 2.00 kg (0.00 ± 11.00 kg) to 4.30 kg (2.00 ± 12.00 kg).
Holzbauer et al. [32] described 31 patients treated with fat infiltration of the TM joint after a follow-up period of 5.1 years. They reported a tendency of surgical conversion after the lipofilling, so that 61% of 31 initially infiltrated patients could be studied in this chapter. An important result of this study is that smoking have a significantly higher risk for therapy failure.
4. Discussion
Since the inception of autologous lipoaspirated fat transplantation as a therapy for osteoarthritis (OA) of the trapeziometacarpal joint [23] numerous research groups have explored this innovative approach involving the injection of autologous fat. Zuk et al. [33] were the first to describe the presence of mesenchymal stem cells in adipose tissue in 2001. The mesenchymal stem cells have regenerative abilities and a potential to differentiate into multiple cell types, which is comparable to bone marrow mesenchymal stem cells [1, 2, 3, 4]. Adipose-derived SVF obtained through enzymatic digestion and centrifugation of collected fat tissue has gained significant popularity for clinical applications in joints displaying osteoarthritic changes [6, 7, 8, 9]. This SVF comprises a diverse cellular composition, including mesenchymal stem cells, endothelial progenitor cells, pericytes and immune cells. It shows strong regenerative potential and the possibility of synergistic impact on immunomodulation, inflammation, and angiogenesis. Adipose-derived stem cells (ASCs) are typically extracted from the stromal vascular fraction (SVF) of adipose tissue. Their morphology is similar to fibroblasts and shows positivity for common mesenchymal stem cell (MSC) markers such as CD44, CD73, CD90 and CD105, while lacking expression of typical hematopoietic markers such as CD14, CD34 and CD45 [10, 12, 33]. Like MSCs, ASCs have the ability to differentiate into various lineages, including osteogenic, adipogenic, myogenic and chondrogenic [12]. Regenerative fat cells exert their regenerative effects primarily through paracrine action [34]. They secrete bioactive molecules, such as cytokines and growth factors, which affect neighboring cells and tissues. These molecules can promote angiogenesis, reduce inflammation and modulate the immune system [12, 13, 14]. Adipose-derived exosomes, which are small vesicles secreted by adipose stem cells, contain various bioactive molecules, including proteins and microRNAs. Studies have shown that adipose-derived exosomes have anti-inflammatory and tissue regenerative effects [35].
The examined studies on intra-articular autologous fat injection for basal thumb and finger osteoarthritis are somewhat limited, but their results are undeniably positive with a great potential for treatment for many years. The injection of autologous fat into the joint consistently led to a reduction in pain and subsequent improvements in hand function. However, when it comes to grip and pinch strength, the outcomes were not consistent but there is a trend to an improvement 12 months after treatment.
Intra-articular injections of cortisone or hyaluronic acid serve as alternative approaches to the liparthroplasty. It’s important not to underestimate the potential chondral damage resulting from repeated cortisone injections [3, 5]. With the liparthroplasty, several other surgical treatments remain available. Autologous fat transfer seems to be a secure and minimally invasive technique that does not burn any bridge to other techniques.
5. Conclusion
Fat grafting and adipose-derived cellular therapies can be effective in finger and thumb osteoarthritis treatment due to their biological and immunomodulatory characteristics. Although basic research provides evidence of these proprieties of adipose-derived stem cells [9, 10, 11, 12, 13, 14], the exact mode of action of liparthroplasty is still not clear. Adipose tissue can provide a cushioning effect due to its ability to absorb and distribute mechanical forces. Based on the findings of this analysis, autologous fat injections into the affected finger joint seem to alleviate pain and enhance hand function. Further investigations should concentrate on identifying the most effective method for processing fat, enhancing the biological qualities and effectiveness of the injected cells. It will be imperative to conduct randomized controlled trials to ascertain whether the injection of autologous fat grafting could significantly contribute to the symptomatic treatment of thumb and finger osteoarthritis.
References
- 1.
Bühler M, Chapple CM, Stebbings S, Pōtiki-Bryant K, David BG. Impact of thumb carpometacarpal joint osteoarthritis: A pragmatic qualitative study. Arthritis Care Research (Hoboken). 2021; 73 (3):336-346 - 2.
Riley N, Vella-Baldacchino M, Thurley N, Hopewell S, Carr AJ, Dean BJF. Injection therapy for base of thumb osteoarthritis: A systematic review and meta-analysis. BMJ Open. 2019; 9 :e027507 - 3.
Wernecke C, Braun HJ, Dragoo JL. The effect of intra-articular corticosteroids on articular cartilage: A systematic review. Orthopedic Journal of Sports Medicine. 2015; 3 (5) - 4.
Suntiparpluacha M, Tammachote N, Tammachote R. Triamcinolone acetonide reduces viability, induces oxidative stress, and alters gene expressions of human chondrocytes. European Review for Medical and Pharmacological Sciences. 2016; 20 :4985-4992 - 5.
Zhang Y, Chen X, Tong Y, Luo J, Bi Q. Development and Prospect of intra-articular injection in the treatment of osteoarthritis: A review. Journal of Pain Research. 2020; 13 :1941-1955 - 6.
Qureshi MK, Halim UA, Khaled AS, Roche SJ, Arshad MS. Trapeziectomy with ligament reconstruction and tendon interposition versus trapeziometacarpal joint replacement for thumb carpometacarpal osteoarthritis: A systematic review and meta-analysis. Journal of Wrist Surgery. 2022; 11 :272-278 - 7.
Holme TJ, Karbowiak M, Clements J, Sharma R, Craik J, Ellahee N. Thumb CMCJ prosthetic total joint replacement: A systematic review. EFORT Open Review. 2021; 6 :316-330 - 8.
Raj S, Clay R, Ramji S, Shaunak R, Dadrewalla A, Sinha V, et al. Trapeziectomy versus joint replacement for first carpometacarpal (CMC 1) joint osteoarthritis: A systematic review and meta-analysis. European Journal of Orthopaedic Surgery and Traumatology. 2022; 32 (6):1001-1021 - 9.
Jo CH, Lee YG, Shin WH, Kim H, Chai JW, Jeong EC, et al. Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee. A proof of concept clinical trial. Stem Cells. 2014; 32 :1254-1266 - 10.
Bora P, Majumdar AS. Adipose tissue-derived stromal vascular fraction in regenerative medicine: A brief review on biology and translation. Stem Cell Research & Therapy. 2017; 8 :145 - 11.
ter Huurne M, Schelbergen R, Blattes R, Blom A, de Munter W, Grevers LC, et al. Antiinflammatory and chondroprotective effects of intraarticular injection of adipose-derived stem cells in experimental osteoarthritis. Arthritis and Rheumatism. 2012; 64 :3604-3613 - 12.
Gimble JM, Katz AJ, Bunnell BA. Adipose-derived stem cells for regenerative medicine. Circulation Research. 2007; 100 :1249-1260 - 13.
Michalek J, Moster R, Lukac L, Proefrock K, Petrasovic M, Rybar J, et al. Stromal vascular fraction cells of adipose and connective tissue in people with osteoarthritis: A case control prospective multi-centric non-randomized study. Global Surgery. 2017; 3 :1-9 - 14.
Feisst V, Meidinger S, Locke MB. From bench to bedside: Use of human adipose-derived stem cells. Stem Cells Cloning. 2015; 8 :149-162 - 15.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ. 2009; 339 :b2700 - 16.
Coleman SR. Structural fat grafts. Clinics in Plastic Surgery. 2001; 28 :111-119 - 17.
Strong AL, Cederna PS, Rubin JP, Coleman SR, Levi B. The current state of fat grafting: A review of harvesting, processing, and injection techniques. Plastic and Reconstructive Surgery. 2015; 136 (4):897-912 - 18.
Pulsfort AK, Wolter TP, Pallua N. The effect of centrifugal forces on viability of adipocytes in centrifuged lipoaspirates. Annals of Plastic Surgery. 2011; 66 (3):292-295 - 19.
Fisher C, Grahovac TL, Schafer ME, Shippert RD, Marra KG, Rubin JP. Comparison of harvest and processing techniques for fat grafting and adipose stem cell isolation. Plastic and Reconstructive Surgery. 2013; 132 :351-361 - 20.
Rose JG, Lucarelli MJ, Lemke BN, et al. Histologic comparison of autologous fat processing methods. Ophthalmic Plastic and Reconstructive Surgery. 2006; 22 :195-200 - 21.
Zhu M, Zhou Z, Chen Y, et al. Supplementation of fat grafts with adipose-derived regenerative cells improves long-term graft retention. Annals of Plastic Surgery. 2010; 64 :222-228 - 22.
Pfaff M, Wu W, Zellner E, Steinbacher DM. Processing technique for lipofilling influences adipose-derived stem cell concentration and cell viability in lipoaspirate. Aesthetic Plastic Surgery. 2014; 38 :224-229 - 23.
Herold C, Fleischer O, Allert S. Eigenfettinjektion in das Sattelgelenk zur Behandlung der Rhizarthrose—eine viel ver- sprechende Therapieoption. Handchirurgie, Mikrochirurgie, Plastische Chirurgie. 2014; 46 :108-112 - 24.
Bohr S, Rennekampff HO, Pallua N. Cell-enriched Lipoaspirate arthroplasty: A novel approach to first carpometacarpal joint arthritis. Hand Surgery. 2015; 20 :479-481 - 25.
Herold C, Rennekampff HO, Groddeck R, Allert S. Autologous fat transfer for thumb carpometacarpal joint osteoarthritis: A prospective study. Plastic and Reconstructive Surgery. 2017; 140 :327-335 - 26.
Haas EM, Volkmer E, Giunta RE. Pilotstudie über die Wirkung und den Nutzen von autologen Fettgewebstransplantaten bei Rhizarthrose verglichen mit einer Kortisoninjektion—3 Monatsergebnisse. Handchirurgie, Mikrochirurgie, Plastische Chirurgie. 2017; 49 :288-296 - 27.
Erne HC, Cerny MK, Ehrl D, Bauer AT, Schmauss V, Moog P, et al. Autologous fat injection versus Lundborg resection arthroplasty for the treatment of Trapeziometacarpal joint osteoarthritis. Plastic and Reconstructive Surgery. 2018; 141 :119-124 - 28.
Haas EM, Eisele A, Arnoldi A, Paolini M, Ehrl D, Volkmer E, et al. One-year outcomes of Intraarticular fat transplantation for thumb carpometacarpal joint osteoarthritis: Case review of 99 joints. Plastic and Reconstructive Surgery. 2020; 145 :151-159 - 29.
Froschauer SM, Holzbauer M, Wenny R, Schmidt M, Huemer GM, Kwasny O, et al. Autologous fat transplantation for thumb carpometacarpal joint osteoarthritis (Liparthroplasty): A case series with two years of follow-UP. Journal of Clinical Medicine. 2020; 10 :113 - 30.
Herold C, Lange J, Rennekampff HO, Allert S, Meyer Marcotty M. Eigenfettinjektion bei Rhizarthrose: 5 Jahresergebnisse bei 42 Patienten. Z. Orthop. Unfall. 2022 - 31.
Meyer-Marcotty M, Batsilas I, Sanders A, Dahmann S, Happe C, Herold C. Lipofilling in osteoarthritis of the finger joints: Initial prospective long-term results. Plastic and Reconstructive Surgery. 2022; 149 (5):1139-1145 - 32.
Holzbauer M, Hopfner M, Haslhofer D, Kwasny O, Duscher D, Froschauer SM. Radial and palmar active range of motion measurement: Reliability of six methods in healthy adults. Journal of Plastic Surgery and Hand Surgery. 2021; 55 :41-47 - 33.
Zuk PA, Zhu M, Ashjian P, De Ugarte DA, Huang JI, Mizuno H, et al. Human adipose tissue is a source of multipotent stem cells. Molecular Biology of the Cell. 2002; 13 (12):4279-4295 - 34.
Trzyna A, Banaś-Ząbczyk A. Adipose-derived stem cells Secretome and its potential application in “stem cell-free therapy”. Biomolecules. 2021; 11 (6):878 - 35.
Heo JS, Kim S, Yang CE, Choi Y, Song SY, Kim HO. Human adipose mesenchymal stem cell-derived exosomes: A key player in wound healing. Tissue Engineering and Regenerative Medicine. 2021; 18 (4):537-548