Abstract
This chapter focuses on the impact of aging on synovial joint function, specifically the changes that occur in joint structure and their implications for mobility. These age-related changes can lead to joint degeneration, decreased joint flexibility, and increased susceptibility to injury or conditions like osteoarthritis. Furthermore, the chapter discusses the consequences of these structural changes on mobility and functional abilities in older individuals. The gradual decline in joint function due to aging can result in limitations in range of motion, joint stiffness, reduced muscle strength, and overall decreased mobility. The implications of these changes on activities of daily living and quality of life are explored, highlighting the importance of maintaining joint health and promoting active lifestyles in older adults. Additionally, the chapter touches upon potential strategies and interventions to mitigate the impact of aging on synovial joint function. It covers approaches such as exercise programs, physical therapy, nutritional considerations, and joint-specific interventions that can help optimize joint health, enhance mobility, and potentially slow down the progression of age-related joint degeneration. Understanding the structural changes that occur in synovial joints with aging and their consequences for mobility is vital for healthcare professionals, researchers, and individuals seeking to promote healthy aging and maintain joint function throughout the lifespan.
Keywords
- synovial joints
- aging
- joint physiology
- physical interventions
- chronic inflammation
1. Introduction
Aging is a natural biological progression that triggers various physiological transformations, notably impacting the musculoskeletal system. Changes in the structure of synovial joints assume a pivotal role in shaping an individual’s mobility and overall well-being [1]. These joints, essential for facilitating movement and offering mechanical support, undergo a sequence of modifications during aging. Such alterations entail intricate interactions among structural elements like cartilage, synovial fluid, ligaments, and the joint capsule, resulting in decreased joint function [2].
Grasping the complex association between aging and synovial joint function is crucial for comprehending the mechanisms underlying age-related constraints on mobility and disorders associated with joints. This chapter explores the multifaceted dimensions of the aging process and its consequences for the structure and function of synovial joints [3]. By meticulously examining the specific structural changes that transpire within these joints, the aim is to uncover the repercussions of these modifications on an individual’s mobility and ability to carry out daily activities independently [4, 5, 6]. Additionally, the chapter will assess the implications of these age-related changes in synovial joints for developing preventive and therapeutic interventions, with the explicit objective of enhancing the quality of life for the aging population. Employing an extensive analysis of relevant literature and recent advancements in the field, the ultimate goal is to provide a comprehensive understanding of the intricate interplay between aging, synovial joint structure, and mobility, fostering enhanced management and care for individuals experiencing age-related deterioration in joint function [1, 3].
2. The anatomy of synovial joints: a foundation for understanding age-related modifications
The anatomy of synovial joints constitutes a foundational understanding crucial for comprehending the modifications that occur with aging and their subsequent impact on joint function. Synovial joints are the most common type of joint in the human body, characterized by their capacity for a wide range of motion. They are essential for facilitating various movements, such as flexion, extension, abduction, adduction, and rotation. Understanding the intricate structures within these joints provides insights into the complex mechanisms underlying age-related changes and their effects on joint health and function [3].
2.1 Articular cartilage
The articular cartilage covers the bone ends within the joint, serving as a smooth and resilient tissue that reduces friction and facilitates smooth movement between the articulating surfaces. Composed of specialized cells called chondrocytes embedded in an extracellular matrix, articular cartilage lacks a direct blood supply and nerve innervation. With advancing age, the articular cartilage undergoes structural changes, including thinning, loss of elasticity, and increased fibrillation and fissuring. These alterations can lead to reduced shock absorption, increased susceptibility to damage, and the development of degenerative joint conditions such as osteoarthritis [4, 5].
2.2 Synovial fluid
Synovial fluid is a viscous, transparent fluid that fills the synovial cavity within the joint, providing lubrication and nourishment to the articular cartilage. It also serves to reduce friction during joint movements. With age, the composition and viscosity of synovial fluid may change, leading to alterations in its lubricating properties. These changes can contribute to increased joint surface friction, discomfort, stiffness, and decreased range of motion [6].
2.3 Ligaments and tendons
Ligaments and tendons are crucial connective tissues that stabilize and support synovial joints. Ligaments connect bone to bone, while tendons connect muscle to bone. These structures help to limit excessive joint movement and prevent dislocation. With aging, ligaments and tendons may experience a decrease in tensile strength and elasticity, leading to decreased joint stability and an increased risk of injury [7, 8].
2.4 Joint capsule
The joint capsule is a fibrous, elastic structure that encloses the synovial joint, maintaining its structural integrity and containing the synovial fluid. The capsule comprises an outer fibrous layer and an inner synovial membrane. With age, the flexibility and elasticity of the joint capsule may diminish, leading to a decrease in the joint’s range of motion and flexibility [5].
2.5 Synovial membrane
The synovial membrane lines the inner surface of the joint capsule and is responsible for producing synovial fluid. It plays a crucial role in maintaining a healthy joint environment by supplying nutrients to the articular cartilage and facilitating the removal of metabolic waste products. During the aging process, the synovial membrane may change, leading to the production of inflammatory mediators and an increase in inflammatory responses within the joint. This can contribute to developing joint-related pathologies, such as synovitis and other inflammatory joint conditions [9].
3. Age-associated alterations in synovial fluid composition and their influence on joint performance
Synovial fluid composition changes significantly as individuals age, impacting joint performance and overall health. The composition of synovial fluid, crucial for lubrication and nutrient supply to the joint, is affected by various age-related alterations [10].
3.1 Reduction in lubricating agents
A notable change is the decline in the production of lubricating agents like hyaluronic acid, which is responsible for the viscosity of the synovial fluid. Reduced levels of hyaluronic acid contribute to decreased lubrication between joint surfaces, leading to increased friction and wear within the joint. Consequently, this can result in joint stiffness, discomfort, and restricted range of motion, significantly influencing joint performance and mobility [11].
3.2 Altered protein concentration
Age-related modifications in the concentration of proteins within synovial fluid affect its lubricating and anti-inflammatory properties. Variations in the levels of lubricin, a glycoprotein that minimizes friction between joint surfaces, can lead to diminished joint lubrication and increased vulnerability to mechanical stress. Moreover, changes in the levels of enzymes like matrix metalloproteinases and aggrecanase contribute to the breakdown of extracellular matrix components, accelerating the progression of degenerative joint diseases, such as osteoarthritis [12].
3.3 Imbalance in inflammatory mediators
The equilibrium of inflammatory mediators within synovial fluid is vital for maintaining a healthy joint environment. Age-related alterations can disrupt this balance, leading to an increase in proinflammatory cytokines and a decrease in anti-inflammatory factors. This imbalance contributes to chronic inflammation within the joint, exacerbating joint damage and impairing overall joint performance [13].
Understanding the complex shifts in synovial fluid composition linked to aging is crucial for developing strategies to maintain joint health and function in older adults. Therapeutic methods focused on addressing changes in synovial fluid, including treatments like viscosupplementation and anti-inflammatory therapies, present encouraging avenues to alleviate the negative impacts of aging on joint performance and enhance the overall well-being of individuals facing age-related declines in joint function [14].
4. Structural deteriorations in aging synovial joints and their impact on mobility and flexibility
As individuals age, synovial joints undergo several structural deteriorations, significantly impacting mobility and flexibility. Understanding these changes is crucial for addressing the challenges faced by the aging population in maintaining functional independence and high quality of life [11, 12, 13].
4.1 Cartilage degeneration
One of the primary structural deteriorations is the degeneration of articular cartilage, which experiences a loss of elasticity and thinning with age. This degeneration reduces the smooth gliding of joint surfaces, leading to increased friction and discomfort during movement. As cartilage deteriorates, joint mobility diminishes, causing stiffness and reduced flexibility, limiting an individual’s range of motion [15].
4.2 Ligament and tendon stiffness
With advancing age, ligaments and tendons lose their elasticity and become stiffer, impacting joint stability and flexibility. Reduced flexibility in these connective tissues can lead to a higher risk of injuries as the joints become less adept at absorbing impact and shock. The loss of flexibility in ligaments and tendons contributes to a decreased overall range of motion, affecting mobility and making movements more challenging for older individuals [16].
4.3 Changes in joint capsule elasticity
The joint capsule, a fibrous structure that encloses the synovial joint, changes elasticity and flexibility due to aging. This alteration limits the joint’s ability to move freely, decreasing mobility and flexibility. The reduced elasticity of the joint capsule can result in joint stiffness and discomfort, further restricting the range of motion and making routine activities more challenging for older people [9, 11].
4.4 Synovial membrane inflammation
The synovial membrane, responsible for producing synovial fluid and maintaining a healthy joint environment, is susceptible to inflammation with age. Chronic inflammation of the synovial membrane can lead to increased production of inflammatory mediators, causing further deterioration of the joint structure. Inflammation in the synovial membrane can result in pain, swelling, and reduced mobility, significantly impacting an individual’s flexibility and ability to perform daily activities [17].
5. Inflammatory responses and their role in accelerating age-related decline in synovial joint function
Inflammatory responses are critical in accelerating age-related decline in synovial joint function. As individuals age, the balance of inflammatory processes within the synovial joints can be disrupted, leading to chronic inflammation and various joint-related disorders. Understanding the impact of inflammatory responses is crucial for comprehending the underlying mechanisms of age-related joint degeneration and developing effective strategies to manage and alleviate the associated symptoms [18].
5.1 The role of chronic inflammation
Chronic low-grade inflammation, often called “inflamm-aging, “is a hallmark of the aging process and is closely linked to the degeneration of synovial joints. Persistent inflammation within the synovial membrane can lead to the release of proinflammatory cytokines and enzymes, which contribute to the breakdown of cartilage and other joint tissues. This chronic inflammatory state can perpetuate a cycle of tissue damage and repair, ultimately accelerating the deterioration of the joint structure [11, 19].
5.2 Impact on synovial fluid composition
Inflammatory responses can also influence the composition of synovial fluid. Elevated levels of inflammatory mediators within the synovial fluid can disrupt the balance of lubricating agents and enzymes, leading to decreased viscosity and impaired lubrication. This alteration in synovial fluid composition can increase joint surface friction, leading to pain, stiffness, and reduced mobility [19].
5.3 Effects on joint capsule and ligaments
Inflammation can affect the integrity of the joint capsule and surrounding ligaments, leading to a loss of elasticity and increased stiffness. Decreased flexibility and range of motion can significantly impact joint function and mobility. Moreover, chronic inflammation can promote the formation of adhesions within the joint capsule, further restricting joint movement and exacerbating the overall decline in joint function [20].
5.4 Role in the development of degenerative joint diseases
Chronic inflammatory responses within synovial joints are closely associated with the development and progression of degenerative joint diseases, such as osteoarthritis and rheumatoid arthritis. Inflammatory mediators can trigger the release of enzymes that degrade cartilage and bone, leading to the erosion of joint surfaces and the development of pain, swelling, and deformity. The resulting joint damage can severely compromise joint function and significantly limit an individual’s mobility and overall quality of life (Figure 1) [17, 18, 19, 20].
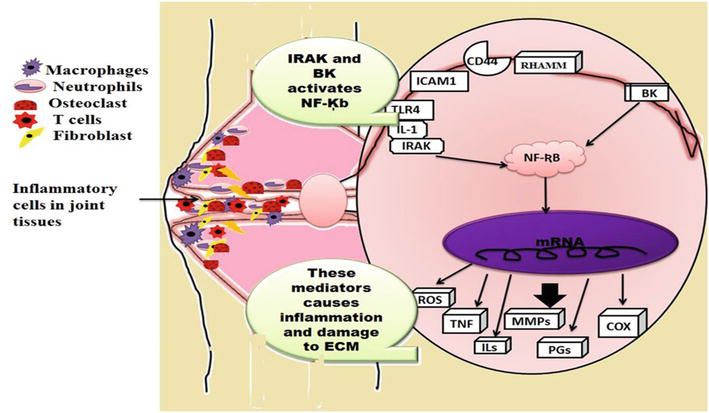
Figure 1.
Role of inflammation in degenerating synovial joints.
6. Implications for mobility and strategies for maintaining joint health in the aging population
The implications for mobility and strategies for maintaining joint health in the aging population are paramount, considering the significant impact of age-related changes on musculoskeletal function. Maintaining mobility is crucial for preserving independence, quality of life, and overall well-being in older individuals. Understanding the implications for mobility and implementing effective strategies for supporting joint health can significantly enhance the overall functional capacity and quality of life in the aging population [21].
As individuals age, various factors, including structural changes in joints, reduced muscle mass, decreased bone density, and alterations in balance and coordination, can collectively contribute to a decline in mobility. Age-related joint degeneration, such as cartilage thinning, ligament stiffness, and inflammation, can result in joint pain, stiffness, and reduced range of motion, significantly impacting mobility. Additionally, decreased muscle strength and flexibility can further exacerbate mobility challenges, leading to daily living difficulties and increasing the risk of falls and injuries [22].
Several strategies can be employed to maintain joint health and improve mobility in the aging population [23]. These strategies include:
6.1 Regular physical activity
Regular physical activity, including low-impact walking, swimming, and cycling, can help improve joint flexibility, muscle strength, and overall mobility. Exercise programs focused on improving balance and flexibility, such as yoga and tai chi, can also be beneficial for maintaining joint health [11, 13, 20]. Engaging in strength-training exercises helps build muscle mass and strength, providing better support and stability for the joints. Strengthening the muscles around the joints, including the quadriceps, hamstrings, and core muscles, can help alleviate the pressure on the joints, reducing the risk of joint injuries and enhancing overall joint function [21]. Physical activity stimulates the production of synovial fluid, which acts as a lubricant for the joints, promoting smoother and more efficient movement. Regular movement helps nourish the cartilage by facilitating the exchange of nutrients and waste products, thereby enabling the overall health and longevity of the joint cartilage [22]. When combined with a balanced diet, regular physical activity can aid in weight management, reducing the strain on weight-bearing joints such as the hips, knees, and ankles. Maintaining a healthy weight helps minimize the risk of developing joint-related conditions such as osteoarthritis, as excess body weight can exacerbate joint pain and accelerate the deterioration of joint structures [23]. Physical activity improves blood circulation, delivering essential nutrients and oxygen to the joints and promoting overall health and function. Improved circulation also aids in the removal of waste products and inflammatory mediators from the joints, reducing the risk of inflammation and supporting the body’s natural healing processes [24]. Regular physical activity improves mood, reduces stress levels, and enhances overall well-being. The psychological benefits of exercise can contribute to better pain management, increased motivation to adhere to an active lifestyle, and improved quality of life, promoting a holistic approach to joint health and overall wellness [2, 9].
6.2 Healthy weight management
Maintaining a healthy weight is crucial for reducing the strain on joints, particularly weight-bearing joints such as the knees and hips. Excess body weight can accelerate joint degeneration and increase the risk of developing osteoarthritis, a condition characterized by the breakdown of joint cartilage [25]. By managing body weight within a healthy range, individuals can minimize the strain on their joints, reducing the likelihood of joint pain and improving overall joint function. Weight management strategies, including a balanced diet and portion control, can help alleviate joint pressure and minimize the risk of joint-related complications [26]. Maintaining a healthy weight reduces the strain on the joints and improves overall physical function and mobility. Individuals with a healthy body weight often experience improved flexibility, agility, and balance, enabling them to engage in various physical activities and daily tasks without experiencing excessive joint discomfort or limitations [27].
Healthy weight management encourages individuals to adopt a balanced and nutritious diet rich in essential vitamins, minerals, and antioxidants. Consuming a diet that includes a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats can support joint health by providing the necessary nutrients for maintaining the integrity of joint structures and promoting overall musculoskeletal well-being. Healthy weight management contributes to an improved quality of life, as it helps individuals maintain their independence, engage in various activities, and experience fewer limitations related to joint health. By promoting a healthy weight, individuals can enjoy a better overall sense of well-being, reduced pain, and improved mobility, leading to a more active and fulfilling lifestyle [16, 19].
6.3 Essential nutrients for joint health
A well-balanced diet rich in essential nutrients, including vitamins, minerals, and antioxidants, can support joint health and reduce the risk of inflammation and oxidative stress. Including foods with anti-inflammatory properties, such as fatty fish, fruits, vegetables, and whole grains, can help mitigate the impact of inflammation on joint function [12].
6.3.1 Omega-3 fatty acids
Found in fatty fish such as salmon, mackerel, and sardines, as well as in flaxseeds and chia seeds, omega-3 fatty acids possess potent anti-inflammatory properties. These nutrients can help reduce joint stiffness and alleviate symptoms associated with inflammatory joint conditions such as rheumatoid arthritis [10].
6.3.2 Vitamin D
Essential for maintaining bone health, vitamin D is crucial in calcium absorption and mineralization. Sunlight exposure, fortified dairy products, and certain fish species are excellent sources of vitamin D, which can help prevent the development of osteoporosis and support overall joint integrity [14].
6.3.3 Calcium and magnesium
Crucial minerals for bone health. Calcium and magnesium help maintain bone density and strength, reducing the risk of fractures and osteoporosis. Dairy products, leafy green vegetables, nuts, and seeds are excellent sources of these minerals, supporting overall bone and joint health [7, 9].
6.3.4 Antioxidants
Abundant in fruits and vegetables, antioxidants such as vitamins C and E help neutralize free radicals, reducing oxidative stress and inflammation. Various colorful fruits and vegetables can provide a rich source of antioxidants, promoting joint health and protecting against joint-related conditions [16, 21].
6.3.5 Anti-inflammatory foods
Certain foods possess anti-inflammatory properties that help alleviate joint pain and reduce inflammation. Incorporating foods such as berries, cherries, turmeric, ginger, and green tea into the diet can help mitigate the symptoms of inflammatory joint disorders and promote overall joint health [20].
6.3.6 Hydration
Maintaining adequate hydration is crucial for joint health, as water helps hydrate and nourish the cartilage within the joints. Staying properly hydrated supports the smooth movement of joints and helps prevent the onset of conditions such as gout, which can be exacerbated by dehydration [6, 9].
6.3.7 Balanced diet for overall well-being
Emphasizing a balanced diet that includes a variety of whole grains, lean proteins, healthy fats, and a colorful array of fruits and vegetables is vital for promoting overall musculoskeletal well-being. A well-rounded diet provides the necessary nutrients for maintaining joint integrity, reducing the risk of inflammation and oxidative stress, and supporting overall joint health and mobility [1, 9].
6.4 Joint-friendly lifestyle modifications
Joint-friendly lifestyle modifications are essential for promoting and maintaining optimal joint health, particularly in individuals experiencing age-related changes or those with preexisting joint conditions. These modifications encompass various adjustments to daily activities and habits that help minimize stress on the joints, reduce the risk of injury, and alleviate joint pain [11].
6.4.1 Proper body mechanics
Adopting proper body mechanics during daily activities, such as lifting, carrying, and bending, can significantly reduce joint strain. Using the appropriate techniques, such as lifting with the legs rather than the back, can help prevent injuries, especially to the spine, hips, and knees. Maintaining proper posture while sitting, standing, and walking is also essential for reducing unnecessary stress on the spine and promoting optimal joint alignment [20].
6.4.2 Ergonomic adjustments
Making ergonomic adjustments in the home and workplace can help reduce joint strain and improve overall comfort. Using supportive chairs with proper back and armrests, adjusting the height of workstations to promote good posture, and using ergonomic tools and devices that reduce repetitive strain on the joints can significantly contribute to minimizing joint discomfort and promoting musculoskeletal health [7, 10].
6.4.3 Low-impact exercise
Engaging in low-impact exercises, such as swimming, cycling, and using elliptical machines, can help improve joint flexibility and muscle strength without placing excessive stress on the joints. These exercises promote cardiovascular health, enhance joint mobility, and support overall physical function, making them ideal for individuals with joint-related conditions or those looking to prevent joint injuries [11, 20].
6.4.4 Joint protection during physical activities
Implementing proper joint protection techniques during physical activities, such as wearing appropriate protective gear during sports or using joint-supporting braces or wraps, can help minimize the risk of joint injuries. Additionally, using the correct footwear with adequate arch support and cushioning can reduce the impact on the joints during walking, running, or other weight-bearing activities [21].
6.4.5 Avoidance of repetitive joint movements
Limiting repetitive joint movements and avoiding activities that place excessive strain on the joints can help prevent the development or exacerbation of joint-related conditions such as tendonitis or bursitis. Regular breaks during repetitive tasks and incorporating variety into daily activities can reduce the risk of overuse injuries and support long-term joint health [28].
6.4.6 Assistive devices and mobility aids
Using assistive devices and mobility aids, such as canes, walkers, and grab bars, can provide additional support and stability, particularly for individuals with mobility issues or those at a higher risk of falls. These devices help reduce the pressure on the joints, promote safer movement, and enhance overall functional independence [26].
6.5 Medical interventions and therapies
Seeking appropriate medical interventions, including physical therapy, pain management, and joint-preserving surgeries, can help alleviate joint pain, improve mobility, and enhance overall joint health and function [22].
6.6 Physical therapy
Physical therapy is a fundamental component of joint health management, focusing on rehabilitating and strengthening muscles, tendons, and ligaments surrounding the joints [5, 8]. Physical therapists develop customized exercise regimens and treatment plans tailored to the specific needs of individuals, aiming to improve joint flexibility, range of motion, and overall musculoskeletal function. Physical therapy can also help alleviate joint pain, reduce inflammation, and enhance mobility, making it an essential intervention for individuals recovering from joint injuries or those managing chronic joint-related conditions [12, 19].
6.7 Pharmacological interventions
Pharmacological interventions, including the use of nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and disease-modifying antirheumatic drugs (DMARDs), are commonly employed to manage pain, reduce inflammation, and slow the progression of joint-related disorders such as osteoarthritis and rheumatoid arthritis [28]. These medications help alleviate symptoms, improve joint function, and enhance the overall quality of life for individuals experiencing joint discomfort and inflammation [20].
6.7.1 Joint injections
Intra-articular joint injections, such as corticosteroids and hyaluronic acid, provide targeted relief for individuals with inflammatory joint conditions. Corticosteroid injections help reduce inflammation and alleviate pain, while hyaluronic acid injections improve joint lubrication and cushioning, particularly in individuals with osteoarthritis. These injections can provide temporary or long-term relief, depending on the specific needs and conditions of the individual [29].
6.7.2 Joint-preserving surgeries
Surgical interventions, including arthroscopic procedures, joint realignment surgeries, and joint replacement surgeries, are employed to preserve joint function, alleviate pain, and improve overall joint mobility [2]. These surgeries are recommended for individuals with advanced joint degeneration or severe joint-related conditions that have not responded to conservative treatments. Joint-preservation surgeries aim to restore joint integrity, improve range of motion, and enhance the overall quality of life for individuals with debilitating joint conditions [30].
6.8 Complementary and alternative therapies
Complementary and alternative therapies, such as acupuncture, chiropractic care, and massage therapy, are often utilized in conjunction with conventional treatments to provide additional relief for individuals with joint-related discomfort. These therapies focus on promoting relaxation, reducing muscle tension, improving overall joint flexibility, enhancing the effectiveness of conventional medical interventions, and contributing to a comprehensive approach to joint health management [22, 23, 24, 25].
7. Conclusion
In conclusion, this comprehensive exploration of aging and its impact on synovial joint function underscores the intricate interplay between physiological changes, structural modifications, and their implications for mobility and overall joint health. The aging process brings about a series of complex alterations within the synovial joints, including changes in synovial fluid composition, structural deterioration, inflammatory responses, and mobility limitations. These changes significantly contribute to the development and progression of various joint-related disorders, posing significant challenges for the aging population.
Understanding the multifaceted nature of these age-related modifications in synovial joints is paramount in developing effective strategies to preserve joint health and enhance the quality of life for older individuals. Implementing interventions such as regular physical activity, healthy weight management, proper nutrition, joint-friendly lifestyle modifications, and medical interventions and therapies can play a pivotal role in mitigating the adverse effects of aging on joint function and mobility.
Furthermore, fostering a holistic approach to joint health management that integrates preventive measures, personalized treatment plans, and comprehensive care can significantly improve functional independence and overall well-being in the aging population. By emphasizing the importance of early intervention, regular monitoring, and the implementation of evidence-based practices, healthcare professionals can empower individuals to actively participate in optimal joint health, promoting a more active, independent, and fulfilling lifestyle throughout the aging process.
References
- 1.
Loeser RF. Age-related changes in the musculoskeletal system and the development of osteoarthritis. Clinics in Geriatric Medicine. 2010; 26 (3):371-386. DOI: 10.1016/j.cger.2010.03.002 - 2.
Walk RE, Moon HJ, Tang SY, Gupta MC. Contrast-enhanced microCT evaluation of degeneration following partial and full width injuries to the mouse lumbar intervertebral disc. Scientific Reports. 2022; 12 (1):15555. DOI: 10.1038/s41598-022-19487-9 - 3.
Jiongnan X, Shao T, Lou J, Zhang J, Xia C. Aging, cell senescence, the pathogenesis and targeted therapies of intervertebral disc degeneration. Frontiers in Pharmacology. 2023; 14 :1172920. DOI: 10.3389/fphar.2023.1172920 - 4.
Chaganti RK, Parimi N, Cawthon P, et al. Association of 25-hydroxyvitamin D with prevalent osteoarthritis of the hip in elderly men: The osteoporotic fractures in men study. Arthritis and Rheumatism. 2010; 62 (2):511-514 - 5.
He Y, Li Z, Alexander PG, Ocasio-Nieves BD, Yocum L, Lin H, et al. Pathogenesis of osteoarthritis: Risk factors, regulatory pathways in chondrocytes, and experimental models. Biology. 2020; 9 :194. DOI: 10.3390/biology9080194 - 6.
Ohnishi T, Iwasaki N, Sudo H. Causes of and molecular targets for the treatment of intervertebral disc degeneration: A review. Cell. 2022; 11 (3):394. DOI: 10.3390/cells11030394 - 7.
Janockova J, Slovinska L, Harvanova D, Spakova T, Rosocha J. New therapeutic approaches of mesenchymal stem cells-derived exosomes. Journal of Biomedical Science. 2021; 28 (1):39 - 8.
Sekelova T, Danisovic L, Cehakova M. Rejuvenation of senescent mesenchymal stem cells to prevent age-related changes in synovial joints. Cell Transplantation. 2023; 32 :1-17. DOI: 10.1177/09636897231200065 - 9.
Wen P, Zheng B, Zhang B, Ma T, Hao L, Zhang Y. The role of ageing and oxidative stress in intervertebral disc degeneration. Frontiers in Molecular Biosciences. 2022; 9 :1052878. DOI: 10.3389/fmolb.2022.1052878 - 10.
Colbath AC, Frisbie DD, Dow SW, Kisiday JD, Wayne McIlwraith C, Goodrich LR. Equine models for the investigation of mesenchymal stem cell therapies in orthopaedic disease. Operative Techniques in Sports Medicine. 2017; 25 (1):41-49. DOI: 10.1053/j.otsm.2016.12.007 - 11.
Zhang N, Zhu J, Ma Q , Zhao Y, Wang Y, Hu X, et al. Exosomes derived from human umbilical cord MSCs rejuvenate aged MSCs and enhance their functions for myocardial repair. Stem Cell Research & Therapy. 2020; 11 (1):273 - 12.
Tonomura H, Nagae M, Takatori R, Ishibashi H, Itsuji T, Takahashi K. The potential role of hepatocyte growth factor in degenerative disorders of the synovial joint and spine. International Journal of Molecular Sciences. 2020; 21 :8717. DOI: 10.3390/ijms21228717 - 13.
Abed E, Bouvard B, Martineau X, Jouzeau JY, Reboul P, Lajeunesse D. Elevated hepatocyte growth factor levels in osteoarthritis osteoblasts contribute to their altered response to bone morphogenetic protein-2 and reduced mineralization capacity. Bone. 2015; 75 :111-119 - 14.
Frisch RN, Curtis KM, Aenlle KK, Howard GA. Hepatocyte growth factor and alternative splice variants—Expression, regulation and implications in osteogenesis and bone health and repair. Expert Opinion on Therapeutic Targets. 2016; 20 :1087-1098 - 15.
Ishibashi H, Tonomura H, Ikeda T, Nagae M, Sakata M, Fujiwara H, et al. Hepatocyte growth factor/c-met promotes proliferation, suppresses apoptosis, and improves matrix metabolism in rabbit nucleus pulposus cells in vitro . Journal of Orthopaedic Research. 2016;34 :709-716 - 16.
Hang F, Zhao X, Shen H, Zhang C. Molecular mechanisms of cell death in intervertebral disc degeneration (review). International Journal of Molecular Medicine. 2016; 37 :1439-1448 - 17.
Shamji MF, Setton LA, Jarvis W, So S, Chen J, Jing L, et al. Proinflammatory cytokine expression profile in degenerated and herniated human intervertebral disc tissues. Arthritis and Rheumatism. 2010; 62 :1974-1982 - 18.
Zou F, Jiang J, Lu F, Ma X, Xia X, Wang L, et al. Efficacy of intradiscal hepatocyte growth factor injection for the treatment of intervertebral disc degeneration. Molecular Medicine Reports. 2013; 8 :118-122 - 19.
Conaghan PG et al. Impact and therapy of osteoarthritis: The arthritis care OA nation 2012 survey. Clinical Rheumatology. 2015; 34 (9):1581-1588 - 20.
Coryell PR, Diekman BO, Loeser RF. Mechanisms and therapeutic implications of cellular senescence in osteoarthritis. Nature Reviews Rheumatology. 2021; 17 :47-57. DOI: 10.1038/s41584-020-00533-7 - 21.
Allen KD et al. Osteoarthritis: Models for appropriate care across the disease continuum. Best Practice & Research. Clinical Rheumatology. 2016; 30 (3):503-535 - 22.
Vidal-Bralo L et al. Specific premature epigenetic aging of cartilage in osteoarthritis. Aging. 2016; 8 (9):2222-2231 - 23.
Fellows CR, Matta C, Zakany R, Khan IM, Mobasheri A. Adipose, bone marrow and synovial joint-derived mesenchymal stem cells for cartilage repair. Frontiers in Genetics. 2016; 7 :234346. DOI: 10.3389/fgene.2016.00213 - 24.
Luria A, Chu CR. Articular cartilage changes in maturing athletes: New targets for joint rejuvenation. Sports Health. 2014; 6 (1):18-30. DOI: 10.1177/1941738113514369 - 25.
Sekiya I, Muneta T, Horie M, Koga H. Arthroscopic transplantation of synovial stem cells improves clinical outcomes in knees with cartilage defects. Clinical Orthopaedics and Related Research. 2015; 473 :2316-2326. DOI: 10.1007/s11999-015-4324-8 - 26.
Spees JL, Lee RH, Gregory CA. Mechanisms of mesenchymal stem/stromal cell function. Stem Cell Research & Therapy. 2016; 7 :1-13. DOI: 10.1186/s13287-016-0363-7 - 27.
Steward AJ, Kelly DJ. Mechanical regulation of mesenchymal stem cell differentiation. Journal of Anatomy. 2015; 227 :717-731. DOI: 10.1111/joa.12243 - 28.
Trumbull A, Subramanian G, Yildirim-Ayan E. Mechanoresponsive musculoskeletal tissue differentiation of adipose-derived stem cells. Biomedical Engineering Online. 2016; 15 :43. DOI: 10.1186/s12938-016-0150-9 - 29.
Wyles CC, Houdek MT, Behfar A, Sierra RJ. Mesenchymal stem cell therapy for osteoarthritis: Current perspectives. Stem Cells Cloning. 2015; 8 :117-124. DOI: 10.2147/SCCAA.S68073 - 30.
Zhou Q , Li B, Zhao J, Pan W, Xu J, Chen S. IGF-I induces adipose derived mesenchymal cell chondrogenic differentiation in vitro and enhances chondrogenesis in vivo . In Vitro Cellular & Developmental Biology. Animal. 2016;52 :356-364. DOI: 10.1007/s11626-015-9969-9