Objective of reconstruction (In decreasing order) [9].
Abstract
Brachial plexus injuries are semi-emergency conditions that require early intervention. Nerve transfers in adult brachial plexus injuries have become the standard treatment that gives reasonably good results if performed before the degeneration of muscle end plates. A clinical diagnosis based on clinical examinations supported by radiological and electrophysiological investigations is required that guides the specific procedures to be chosen. The surgeons must prioritize the objectives of reconstruction and keeping the different lifeboats for the use in future before choosing a specific nerve transfer. Also, it is important to be familiar with different nerve transfers so that one can select and perform a specific one based on pre-operative examinations and intraoperative findings of nerve stimulations. The author aims to describe the approach for exploring and dissecting the brachial plexus and different surgical techniques of nerve transfers used for different muscle reinnervations in different scenarios.
Keywords
- nerve transfer
- adult brachial plexus injury
- brachial plexus exploration
- nerve transfer for shoulder and elbow function
- reconstruction in brachial plexus
1. Introduction
Brachial plexus injury is one of the most devastating conditions which (if not treated on time), can cause irreversible loss of functions of the upper limb.
Historically, the outcome of surgical interventions in brachial plexus injuries was not very promising until Millesi described the concept of nerve grafting and found that when a nerve is injured, a useful recovery can be achieved by microsurgery if the two ends of the nerve are repaired or reconstructed by nerve graft [1]. Later on, Narakas also showed better results supported by many other brachial plexus surgeons across the world [2]. The surgical management of the brachial plexus has improved over the past few decades due to advancements in microsurgery, a better understanding of nerve regeneration, and nerve coaptation techniques with nerve glue. Although Nerve grafting revolutionized the treatment of brachial plexus injury, this may not be always possible especially when there is root avulsion injury and when the gap between two cut ends of nerves is more.
Nerve transfers in the form of neurotizing the injured nerve or part of the brachial plexus with the healthy, uninjured nerve either intraplexal or extraplexal can give reasonably better results if performed on time. Various nerve surgeons described and evolved various nerve transfers which have become the standard of care in brachial plexus injuries. An earlier description of Neurotization or nerve transfer was described by A. Lurje in 1948 who identified several neurotizers as n. phrenicus, n. thoracalis longus, nn. thoracales anterior can be used to neurotize injured brachial plexus segments [3].
Oberlin in 1994 described using Flexor carpi ulnaris fascicle to neurotize the muscular branch of the musculocutaneous nerve to reinnervate the biceps and found M4 recovery [4]. Later on, it was modified to perform double innervations by coapting median nerve fascicles to the brachialis, the idea originally described by McKinnon [5]. Somsak Leechavengvongs in 2003 described transferring nerve to the long head of triceps to deltoid muscles in upper brachial plexus palsy which has shown excellent recovery of M4 power [6]. Although, the techniques described are simpler, replicable, and often give good results has received worldwide acceptance. But before planning a nerve transfer surgery for the brachial plexus, it is important to understand the integrity of which nerve is lost and which is preserved before planning for neurotization.
2. Nerve transfer
2.1 Prerequisite for successful nerve transfer
The donor nerve or its fascicle to be transferred should be expandable [7, 8].
The coaptation of the nerves from the donor to the recipient should be tension free and any nerve graft should be used selectively and avoided if possible
The transfer should be close to the target muscles
The transferred nerve should be pure motor if the aim of transfer is for motor recovery
Donor nerve should have a maximum number of axons
Early transfer gives better recovery
There should be a complete passive range of motion across the joints before planning the nerve transfer.
2.2 Objective
A complete examination of the brachial plexus, understanding the relevant anatomy (Figure 1) with documentation is important that involves 58 muscles supplied by different nerves of the brachial plexus. Apart from the examination of the brachial plexus proper, it is important to evaluate what are the priorities of reconstruction (Table 1), available donors, and recipient’s nerves to be neurotized to define aims and objectives for nerve transfers (Table 2).
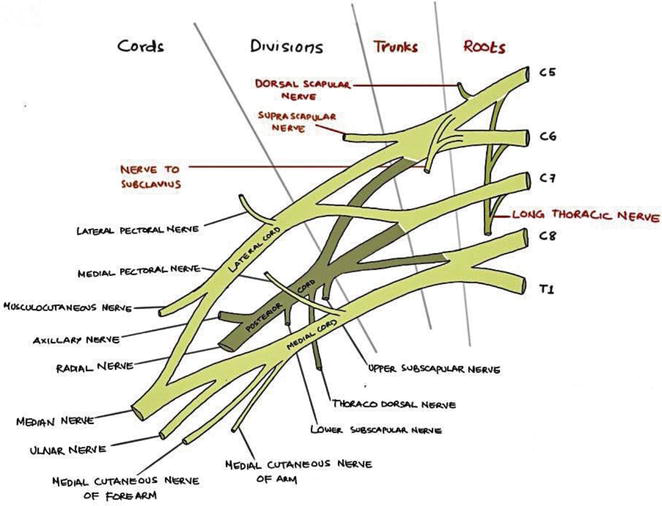
Figure 1.
Schematic diagram of Brachial Plexus (Sketched by Dr Jishnu).
| Elbow flexion |
| Shoulder stability with shoulder abduction and external rotation |
| Hand and wrist flexion |
| Sensation of the hand |
| Elbow extension |
| Wrist & fingers extension |
| Recovery of Intrinsic muscles of hand |
Table 1.
| For Shoulder | For Elbow | For Hand | For Sensation | ||||
|---|---|---|---|---|---|---|---|
| Donor | Recipient | Donor | Recipient | Donor | Recipient | Donor | Recipients |
|
|
|
| CC7 | Median nerve C8,T1 | ICN, Intercosto-brachial nerve, Sensory branch of ICN | Lateral contribution of median nerve |
Table 2.
The different nerve transfers.
SAN, Spinal accessory nerve; SSN, suprascapular nerve; ICN, intercostal nerve; MCN, musculocutaneous nerve; CC7, contralateral C7 nerve.
2.3 Brachial plexus exploration
Brachial plexus is explored
The patient is
2.4 Marking
Suprasternal notch, posterior border of the sternocleidomastoid, and if possible prominence of external jugular vein is marked Figure 2. Supraclavicular brachial plexus can be explored through either a transverse incision or a V-shaped incision. One limb of V is marked at the posterior border of the sternocleidomastoid, whereas the other is marked 1 cm above and parallel to the clavicle.
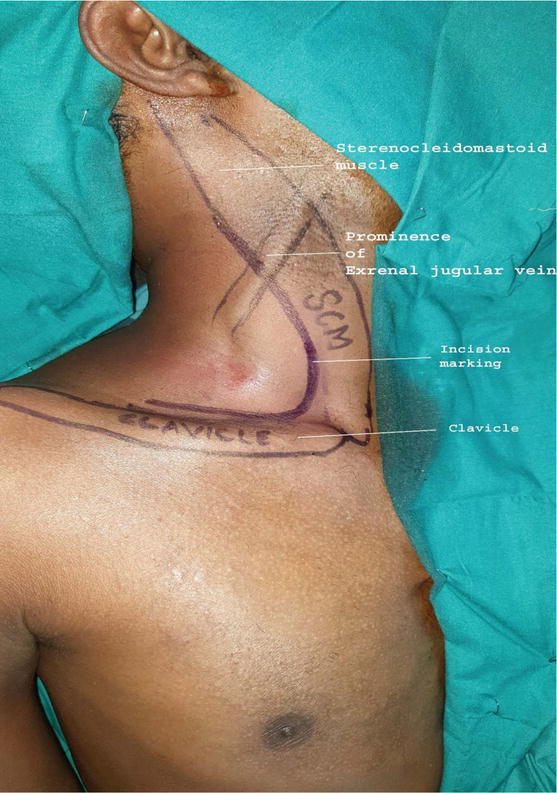
Figure 2.
Marking for exploration of brachial plexus.
The marked incision line is infiltrated with 1:2 lakh adrenaline with saline. Once the incision is made over the marked line, the skin and platysma flap are elevated. In the upper portion of the incision, one will find the external jugular vein which is ligated. In the upper part of the neck, one will encounter several branches of the cervical plexus that may be confused with the spinal accessory nerve (Figure 3).
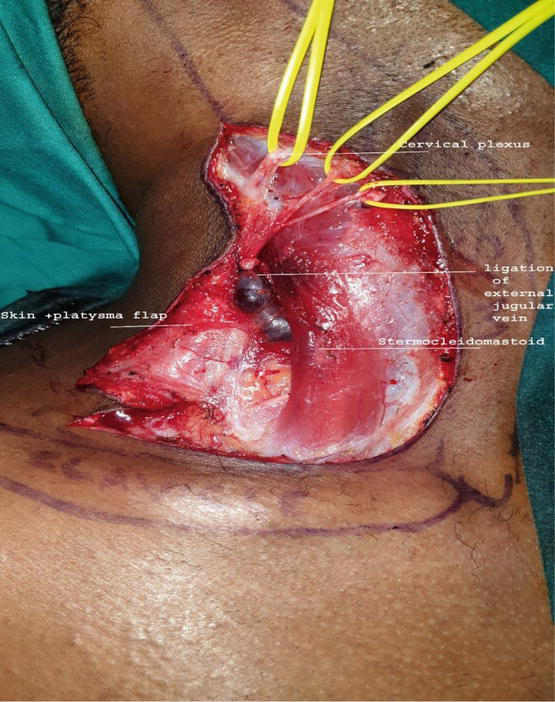
Figure 3.
Raising of skin platysma flap and preservation of cervical plexus.
The spinal accessory nerve arises from the posterior border of the sternocleidomastoid, runs obliquely, and supplies to the trapezius giving multiple branches. In the lower parts, one gets a layer of fatty tissue which is raised as a triangular flap and is sutured back while closing the neck wound to reduce the dead space (Figure 4).
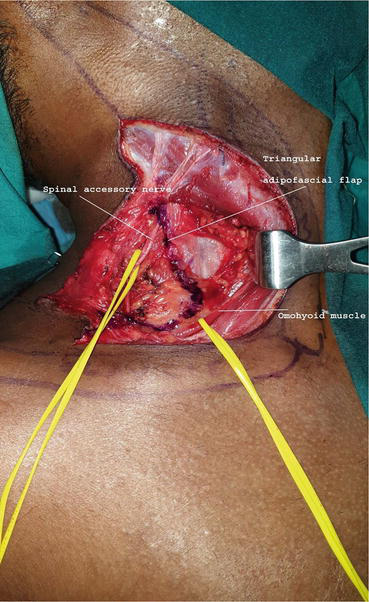
Figure 4.
marking for the adipo-fascial flap, dissection of spinal accessory nerve, and omohyoid muscle in the lower part.
The transverse cervical artery is encountered in the lower part which can be preserved or clipped (Figure 5).
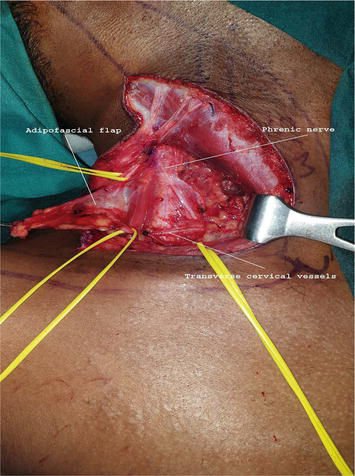
Figure 5.
raising of the adipo-fascial flap, dissecting phrenic nerve and transverse cervical vessels.
The Omohyoid muscle that runs transversely is divided and the first trunk of the brachial plexus is visualized that is upper trunk or the Erb’s point. From the upper trunk, a suprascapular nerve will arise and the upper trunk further divides into anterior and posterior divisions.
On the medial side one can easily identify and dissect the phrenic nerve which runs longitudinally and pierces into the diaphragm, the strong contraction of the diaphragm can be felt when stimulating it. C7 which continues to form the middle trunk is further divided into anterior and posterior divisions. The lower trunk which is formed by roots from C8, T1 which is usually just closer to the subclavian artery also divided into two divisions. The roots, trunks, and divisions lie in supraclavicular regions (Figure 6).
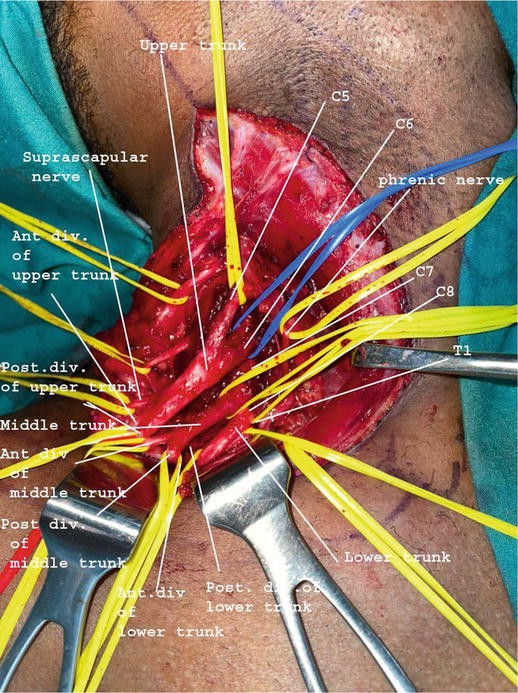
Figure 6.
Supraclavicular brachial plexus with roots, trunk & division.
All the cords are in the infraclavicular region and are named according to their relation with the axillary artery.
The posterior division of all trunks forms the posterior cord which lies posterior to the axillary artery. The anterior division of the upper and middle trunk forms the lateral cord. The anterior division of the lower trunk forms the medial cords. These cords further divided into terminal branches (Figure 7).

Figure 7.
Infraclavicular brachial plexus with its terminal branches.
3. Specific nerve transfer
3.1 For shoulder abduction and stability
3.1.1 Spinal accessory to supra-scapular nerve transfer
3.1.1.1 Relevant anatomy
Spinal accessory nerve is not a part of the brachial plexus and arises from the cranial fossa, it emerges in the proximal part of the sternocleidomastoid and supplies it, then runs in an oblique course and gives several branches to the trapezius.
Whereas suprascapular arises from the upper trunk at Erb’s point, going posteriorly, laterally, and inferiorly to supply supraspinatus and infraspinatus.
3.1.1.2 Exploration and transfer
Spinal accessory nerve transfer can be done during supraclavicular brachial plexus exploration by an anterior approach or via a posterior approach. Each approach has its advantages and disadvantages.
3.1.2 Anterior approach
3.1.2.1 Advantages
No separate incision is required.
Easy to dissect.
3.1.2.2 Disadvantages
In severe injury mainly in case of avulsion or rupture of the upper trunk and C5, and C6 roots of the brachial plexus, the suprascapular nerve displaces more distally and lies below the clavicle where it is difficult to dissect. Also, in case of severe fibrosis of the upper trunk, the suprascapular nerve is either injured or fibrosed, in that case, the posterior approach is preferred. Also, it provides a large future scar on the neck in exploration via the anterior approach.
Many surgeons do not routinely explore the brachial plexus and directly go for distal nerve transfer; in that case, accidental injury to proximal branches of the trapezius can be avoided.
3.1.2.3 Technique
3.1.3 Posterior approach
3.1.3.1 Advantages
3.1.3.2 Disadvantages
The number of axons of the donor ‘spinal accessory nerve’ decreases as it travels distally
Difficult dissection
The patient’s position has to be changed to prone or lateral decubitus during the surgery.
3.1.3.3 Technique
The patient is positioned prone and bony landmarks of the acromion process; the spine of the scapula and midline of the back are marked. The points are joined. The spinal accessory nerve is found at 40% of the distance from the posterior midline and acromion process. The suprascapular nerve is found at the midpoint of the line joining the superior angle of the scapula medially and acromion laterally.
A skin incision is made parallel to the spine of the scapula and the skin flap is raised on both sides. A plane is dissected in between the trapezius and supraspinatus which is delineated by a layer of fatty tissue. Just below the trapezius muscle, the spinal accessory nerve can be identified as supplying it with its branches. It is dissected as far as possible and is cut distally to prepare it for transfer.
The suprascapular nerve is dissected which lies beneath the superior transverse ligament and requires to be divided. Once the ligament is divided, the suprascapular nerve can be dissected and the proximal portion of it is cut which is coapted with a distal portion of the spinal accessory nerve.
3.2 Somsak transfer
Leechavengvongs [6] first reported transferring the nerve to the long heads of the triceps branch of the radial nerve to the anterior branch of the axillary nerve through the posterior approach in 7 patients and achieved M4 power in all patients with an average shoulder abduction of 124 degrees. Later on, it became a reliable procedure addressing the shoulder by reinnervating the deltoid, especially in C5 & C6 brachial plexus injuries with intact C7 roots supplying the triceps. It is done in conditions where the suprascapular nerve is either functional so that deltoid function is superadded with suprascapular nerve or it is combined with SAN to SSN (spinal accessory nerve to suprascapular nerve transfer) transfer for shoulder abduction. Also, it can be done in cases of isolated C5 injury or axillary nerve injury.
3.2.1 Techniques
Somsak transfer is either done in the supine position or a lateral position. The posterior border of the deltoid is marked and a longitudinal incision is made over the posterior aspect of the upper arm. Once the posterior border of the deltoid is delineated it is lifted upward and we get the two divisions of the axillary nerve supplying the deltoid. The axillary nerve arises from the posterior cord, comes out of quadrangular space, and supplies the deltoid. Usually, the anterior division of the deltoid is selected for reinnervation, however, the axillary nerve proper can be used too as the recipient nerve.
Just below the deltoid, triceps muscles will be visualized, the innervations of which can be dissected by lifting one head of the triceps or in between the two heads of the triceps (long and lateral heads). Once we identify the nerve supplying the long head of the triceps, we stimulate it to confirm the contraction of the triceps and isolate it. It is cut distally and is mobilized proximally to coapt with the axillary nerve.
3.2.1.1 Key points (Somsak Transfer)
C5, C6 injury Isolated axillary nerve injury |
|
|
|
|
3.2.1.2 Other nerve transfers for shoulder stability
Thoracodorsal nerve to long thoracic nerve (in patients with winging of the scapula)
Intercostal nerve to anterior branch of axillary nerve or long thoracic nerve
Phrenic nerve to suprascapular nerve transfer
Phrenic nerve to axillary nerve (with nerve graft)
3.3 Elbow flexion
3.3.1 Oberlin transfer
Christopher Oberlin first described the technique of transfer of ulnar nerve fascicle to branch to the musculocutaneous nerve in 1994 in the case of C5, C6 avulsion injury [4]. The simplicity of this procedure and reasonably good results has made this procedure popular and it can be easily replicated by any peripheral nerve surgeon. However, he described choosing any fascicles of the ulnar nerve for transfer. Since at the arm level, the ulnar nerve is usually mixed, so transferring the ulnar nerve fascicle (10%) will result in transferring some motor fibers (10). Later on, other groups suggested fascicles of the nerve supplying the flexor carpi ulnaris which are generally located poster medially to be selected for transfer to a muscular branch of the musculocutaneous nerve (3).
McKinnon [5] described the double fascicular transfer of the FCU fascicle of the ulnar nerve and motor fascicle of the median nerve to the biceps and brachialis of the musculocutaneous. Oberlin included double innervations by coapting the median nerve fascicle to the muscular branch of the brachialis (4). Few people also named it as Oberlin I & 2 transfer (5).
3.3.1.1 Indications
C5 &C6 injury with intact C8 &T1.
3.3.1.2 Technique
Oberlin transfer is performed by making an incision on the medial side of the upper arm which is usually made in the groove that is palpable just below the inferior border of the biceps muscle [4, 5, 9].
Once the skin flap is raised and the medial border of the biceps is delineated, the biceps is elevated. Just below the biceps, we can identify the
The biceps branch usually arises 10–12 cm distal to the acromion [4].
The musculocutaneous nerve travels forward and in the lower parts, it supplies the brachialis muscle by giving a muscular branch to the brachialis before it continues as LABC.
On the more medial side, the ulnar nerve travels anterior to the triceps; intra-fascicular dissection is done under microscope magnification in the proximal aspect slightly lower level than the muscular branch to the biceps. Once donor fascicle (FCU) is identified, which is on the posteromedial aspect toward the surgeon and selected. It is confirmed by intraoperative nerve stimulation. The fascicle is dissected and divided distally and coapted with the biceps muscular branch.
Just medial to the MCN,
In a similar way, the fascicle of the median nerve (either FCR or FDS) is dissected & identified, stimulated by a nerve stimulator, confirmed, and coapted with the muscular branch to the brachialis (Figure 8).
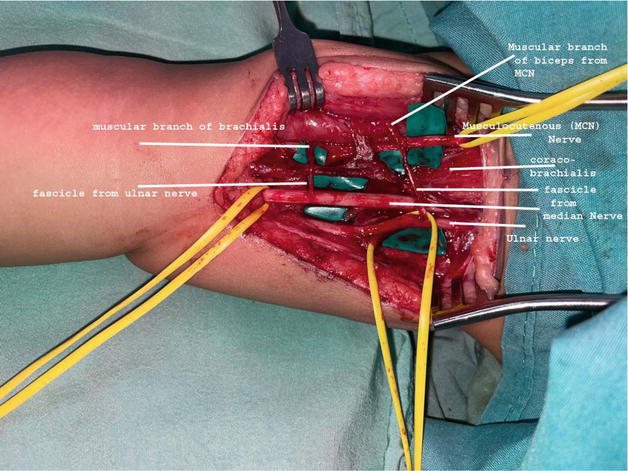
Figure 8.
Oberlin transfer (median nerve fascicle to muscular branch of biceps (from MCN- Musculocutaneous nerve) transfer and Ulnar nerve fascicle to muscular branch of brachialis transfer).
3.3.1.3 Key points (Oberlin Transfer)
|
|
|
|
3.3.2 Intercostal nerve transfer
Intercostal nerve transfer has been used for neurotization of the musculocutaneous nerve as it is out of the zone of the trauma of the brachial plexus (extra plexus) and is frequently available as a donor nerve that is expandable [9]. Apart from neurotizing the musculocutaneous nerve, it can also be used to neurotize the triceps, and deltoid, as a donor for FFMT (Free functioning muscle transfer) or to provide sensation to the hand. It can be used even in cases with a history of rib fracture although one should be cautious in patients with a history of rib fracture, hemothorax, thoracotomy, or phrenic nerve palsy before selecting intercostal nerves as a donor. The commonly used donor is ICN 3,4,5 although from 2nd to 6th ICN can be used.
Relevant anatomy: intercostal nerve runs in the intercostal space on the inferior aspect of the ribs.
3.3.2.1 Technique
The intercostal nerve can be explored through a curvilinear inframammary incision made over the anterior chest wall. This incision is usually connected with the incision in the arm for exploration of the musculocutaneous nerve or incision for the infraclavicular brachial plexus. Once the skin flap is raised, the pectoralis major muscle is retracted and ribs and intercostal muscles are exposed. An incision is made on the anterior surface of the ribs parallel to the upper and lower border with the elevation of the periosteum causing the intercostal nerve to come into the intercostal space which usually lies along the inferior border. It can also be identified by dissecting the sensory branch which lies along the anterior axillary line Careful dissection of intercostal muscles helps in separating the intercostal nerve. It is dissected till the costochondral joint to gain sufficient length to reach the musculocutaneous nerve easily for coaptation without tension. The repair is performed in an abduction position of the shoulder so that there is less risk of its rupture of coaptation during the postoperative period. Care is taken not to injure the pleura during dissection.
Once 2 or 3 intercostal nerves are dissected, they are brought together and connected with the musculocutaneous nerve (Figure 9). Bhandari et al. have described the splint & weld technique [11, 12] for gluing the intercostals nerves.
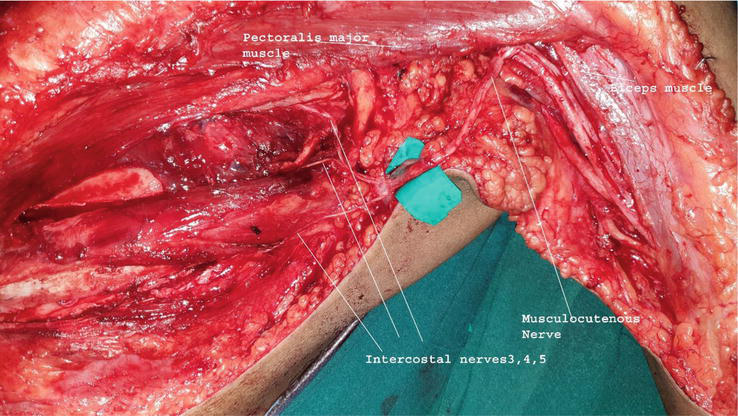
Figure 9.
Intercostal nerve to musculocutaneous nerve transfer.
3.3.2.2 Key points (intercostal nerve to MCN transfer)
|
|
|
|
|
|
|
|
|
|
4. Hand functions
4.1 Contralateral C7 nerve transfer
Contra lateral C7 nerve transfer originally described by Gu [10] in 1989 has been a topic of debate because of many reasons like its route of transfer, relative post-operative weakness of donor’s nerve, and the risk associated with variable outcomes [13, 14]. However, with many studies published with good outcomes, it has been proven to be a safe and useful donor which is expandable because of contributions coming from many spinal roots. Sometimes it is the only option left for addressing hand function especially in pan brachial plexus palsy or for recipient nerve for FFMT.
4.1.1 Technique
The contralateral brachial plexus is explored conventionally on the unaffected side and the C7 nerve root is dissected up to its branches as anterior and posterior divisions. The posterior division is commonly used is divided distally to be transferred as it has more motor axons compared to the anterior division. Half of the C7 nerve fascicles causing pectoralis major contraction are usually chosen and transferred to the ipsilateral side. If we find contraction of hand muscles during intraoperative stimulation, one should not use C7.
After division, a subcutaneous tunnel is created and either a non-vascularized nerve graft (sural nerve) or vascularized ulnar nerve graft (VUNG based on superior ulnar collateral artery & vein) is bridged connecting the cut proximal end of the C7 nerve to another end of the median nerve, suprascapular nerve or musculocutaneous nerve depending upon the reconstruction planned.
The posterior division of contralateral C7 can be brought to the ipsilateral side either with a pre-spinal route, retro-esophageal route, or subcutaneous route to reduce the time taken for axonal regeneration.
4.1.2 Key points (contralateral C7 nerve transfer)
|
|
|
5. Conclusion
Nerve transfer in the brachial plexus has revolutionized the treatment and has become the standard of care to restore useful recovery of upper limb functions in the majority of brachial plexus injuries patients.
The nerve transfers described for shoulder abduction and stability are spinal accessory nerve to supra-scapular nerve transfer which can be superadded with Somsak transfer (using the long head of the triceps branch to the axillary nerve) depending upon the involvement of the C7 root. If hand functions are good, ulnar and median nerve fascicles can be used to neurotize muscular branches of the musculocutaneous nerve to restore elbow flexion. Although intercostal nerves equally give comparable results when used to reinnervate the musculocutaneous nerve, the Spinal accessory nerve or Phrenic nerve are other options that can be considered to neurotize the musculocutaneous nerve. For hand, either contra lateral C7 nerve is used esp. in pan brachial plexus or distal nerve transfer should be considered depending upon the availability of other expandable nerves.
A thorough pre-operative clinical examination, documentation with planning followed by careful intraoperative dissection, microscopic coaptation of nerves, and understanding the regenerating processes of axons with post-operative physiotherapy are keys to the recovery of a good nerve transfer in brachial plexus injuries.
References
- 1.
Millesi H. Surgical management of brachial plexus injuries. The Journal of Hand Surgery. 1977; 2 (5):367-378. DOI: 10.1016/s0363-5023(77)80046-4 - 2.
Narakas AO. The treatment of brachial plexus injuries. International Orthopaedics. 1985; 9 (1):29-36. DOI: 10.1007/BF00267034 - 3.
Lurje A. Concerning surgical treatment of traumatic injury to the upper division of the brachial plexus (Erb's type). Annals of Surgery. 1948; 127 (2):317-326 - 4.
Oberlin C, Béal D, Leechavengvongs S, Salon A, Dauge M, Sarcy J. Nerve transfer to biceps muscle using a part of tulnar nerve for C5–C6 avulsion of the brachial plexus: Anatomical study and report of four cases. The Journal of Hand Surgery. 1994; 19 (2):232-237. DOI: 10.1016/0363-5023(94)90011-6 - 5.
Mackinnon SE, Novak CB, Myckatyn TM, Tung TH. Results of reinnervation of the biceps and brachialis muscles with a double fascicular transfer for elbow flexion. The Journal of Hand Surgery. 2005; 30 (5):978-985. DOI: 10.1016/j.jhsa.2005.05.014 - 6.
Leechavengvongs S, Witoonchart K, Uerpairojkit C, Thuvasethakul P. Nerve transfer to deltoid muscle using the nerve to the long head of the triceps, part II: A report of 7 cases. The Journal of Hand Surgery. 2003; 28 (4):633-638. DOI: 10.1016/s0363-5023(03)00199-0 - 7.
Sinha S, Sharma R, Khani M, Mansari N. Adult brachial plexus injuries: Surgical strategies. In: Mahapatra AK, Midha R, Sinha S, editors. Surgery of Brachial Plexus. Noida, India: Thieme; 2016. pp. 1-12, Chapter 1 - 8.
Bhandari P, Bhatoe H, Mukherjee M, Deb P. Management strategy in post traumatic brachial plexus injuries. The Indian Journal of Neurotrauma. 2012; 9 (1):19-29. DOI: 10.1016/j.ijnt.2012.04.010 - 9.
Spinner RJ, Shin AY, Hebert-Blouin M-N, Elhassan BT, Bishop AT. Traumatic brachial plexus injury. In: Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, editors. Green’s Operative Hand Surgery. 6th ed. Philadelphia: Elsevier. pp. 1235-1291, chapter 38 - 10.
Bhandari PS, Deb P. Posterior approach for both spinal accessory nerve to suprascapular nerve and triceps branch to axillary nerve for upper plexus injuries. The Journal of Hand Surgery. 2013; 38 (1):168-172 - 11.
Bhandari PS. A novel technique in fibrin gluing of intercostal nerves: Splint and weld. Indian Journal of Plastic Surgery: Official Publication of the Association of Plastic Surgeons of India. 2020; 53 (2):298-300. DOI: 10.1055/s-0040-1716430 - 12.
Bhandari PS. Use of fibrin glue in the repair of brachial plexus and peripheral nerve injuries. The Indian Journal of Neurotrauma. 2013; 10 :30-32. DOI: 10.1016/j.ijnt.2013.05.008 - 13.
Gu YD. Cervical nerve root transfer from the healthy side in the treatment of brachial plexus root avulsion. Zhonghua Yi Xue Za Zhi. 1989; 69 (10):563-565 38. Chinese - 14.
Gu YD, Zhang GM, Chen DS, Yan JG, Cheng XM, Chen L. Seventh cervical nerve root transfer from the contralateral healthy side for treatment of brachial plexus root avulsion. The Journal of Hand Surgery. 1992; 17 (5):518-521. DOI: 10.1016/s0266-7681(05)80235-9